Appendectomy
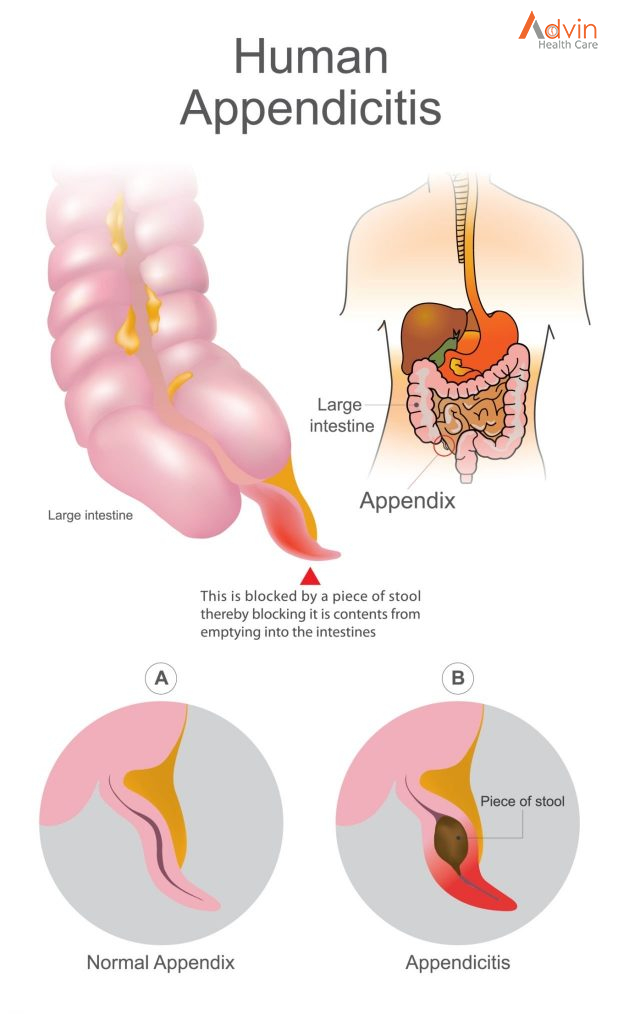
Appendicitis is an inflammation of the appendix, a finger-shaped pouch that projects from your colon on the lower right side of your abdomen.
Appendicitis causes pain in your lower right abdomen. However, in most people, pain begins around the navel and then moves. As inflammation worsens, appendicitis pain typically increases and eventually becomes severe.
Although anyone can develop appendicitis, most often it occurs in people between the ages of 10 and 30. Standard treatment is surgical removal of the appendix.
What Is an Appendectomy?
An appendectomy is the surgical removal of the appendix. It’s a common emergency surgery that’s performed to treat appendicitis, an inflammatory condition of the appendix.
The appendix is a small, tube-shaped pouch attached to your large intestine. It’s located in the lower right side of your abdomen. The exact purpose of the appendix isn’t known. However, it’s believed that it may help us recover from diarrhea, inflammation, and infections of the small and large intestines. These may sound like important functions, but the body can still function properly without an appendix.
When the appendix becomes inflamed and swollen, bacteria can quickly multiply inside the organ and lead to the formation of pus. This buildup of bacteria and pus can cause pain around the belly button that spreads to the lower right section of the abdomen. Walking or coughing can make the pain worse. You may also experience nausea, vomiting, and diarrhea.
It’s important to seek treatment right away if you’re having symptoms of appendicitis. When the condition goes untreated, the appendix can burst (perforated appendix) and release bacteria and other harmful substances into the abdominal cavity. This can be life-threatening, and will lead to a longer hospital stay.
Appendectomy is the standard treatment for appendicitis. It’s crucial to remove the appendix right away, before the appendix can rupture. Once an appendectomy is performed, most people recover quickly and without complications.
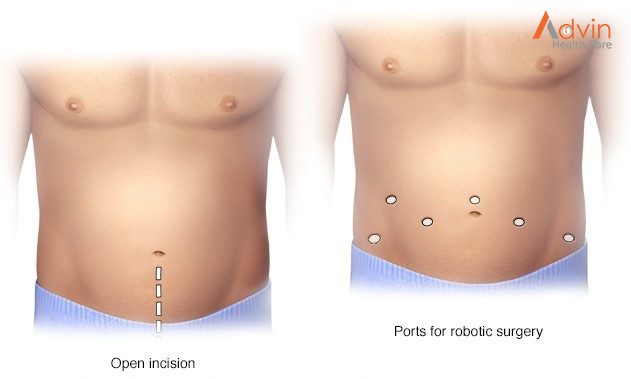
There are 2 types of surgery to remove the appendix. The standard method is an open appendectomy. A newer, less invasive method is a laparoscopic appendectomy.
- Open appendectomy. A cut or incision about 2 to 4 inches long is made in the lower right-hand side of your belly or abdomen. The appendix is taken out through the incision.
- Laparoscopic appendectomy. This method is less invasive. That means it’s done without a large incision. Instead, from 1 to 3 tiny cuts are made. A long, thin tube called a laparoscope is put into one of the incisions. It has a tiny video camera and surgical tools. The surgeon looks at a TV monitor to see inside your abdomen and guide the tools. The appendix is removed through one of the incisions.
During a laparoscopic surgery, your provider may decide that an open appendectomy is needed.
If your appendix has burst and infection has spread, you may need an open appendectomy.
A laparoscopic appendectomy may cause less pain and scarring than an open appendectomy. For either type of surgery, the scar is often hard to see once it has healed.
Both types of surgery have low risk of complications. A laparoscopic appendectomy has a shorter hospital stay, shorter recovery time, and lower infection rates.
Recently, some studies have suggested that intravenous antibiotics alone could cure appendicitis without the need for appendectomy. These results remain controversial and appendectomy remains the standard of care.
What happens during an appendectomy?
In most cases an appendectomy is an emergency surgery and will require a hospital stay. You will have either an open appendectomy or a laparoscopic appendectomy. This will depend on your condition and your healthcare provider’s practices.
An appendectomy is done while you are given medicines to put you into a deep sleep (under general anesthesia).
Generally, the appendectomy follows this process:
- You will be asked to remove any jewelry or other objects that might get in the way during surgery.
- You will be asked to remove your clothing and will be given a gown to wear.
- An IV (intravenous) line will be put in your arm or hand.
- You will be placed on the operating table on your back.
- If there is a lot of hair at the surgical site, it may be clipped off.
- A tube will be put down your throat to help you breathe. The anesthesiologist will check your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
Open appendectomy
- A cut or incision will be made in the lower right part of your belly.
- Your abdominal muscles will be separated and the abdominal area will be opened.
- Your appendix will be tied off with stitches and removed.
- If your appendix has burst or ruptured, your abdomen will be washed out with salt water (saline).
- The lining of your abdomen and your abdominal muscles will be closed with stitches. A small tube may be put in the incision to drain out fluids.
Laparoscopic appendectomy
- A tiny incision will be made for the tube (laparoscope). More cuts may be made so that other tools can be used during surgery.
- Carbon dioxide gas will be used to swell up your abdomen so that your appendix and other organs can be easily seen.
- The laparoscope will be put in and your appendix will be found.
- Your appendix will be tied off with stitches and removed through an incision.
- When the surgery is done, the laparoscope and tools will be removed. The carbon dioxide will be let out through the cuts. A small tube may be placed in the cut to drain out fluids.
Advantages of appendectomy
Results may vary depending upon the type of procedure and patient’s overall condition. Common advantages are:
- Less postoperative pain
- May shorten hospital stay
- May result in a quicker return to bowel function
- Quicker return to normal activity
- Better cosmetic results
Advin Instrument Use In Appendectomy Surgery
- Metzenbaum Scissors TC
- Mayo Scissors TC
- Scalpel Handle
- Allis Tissue Forceps
- Kochers Tissue Forceps
- Mcindoe Forceps
- Babcocks Tissue Forceps
- Mayo Hagar Needle Holder
- Sponge Holding Forceps
- Backhaus Towel Clamps
- Criles Forceps
- Spencer Wells
- U S Army Retractor
- Adson Forceps
- Gallipots
- Kidney Dish
- Multifunction Trocar
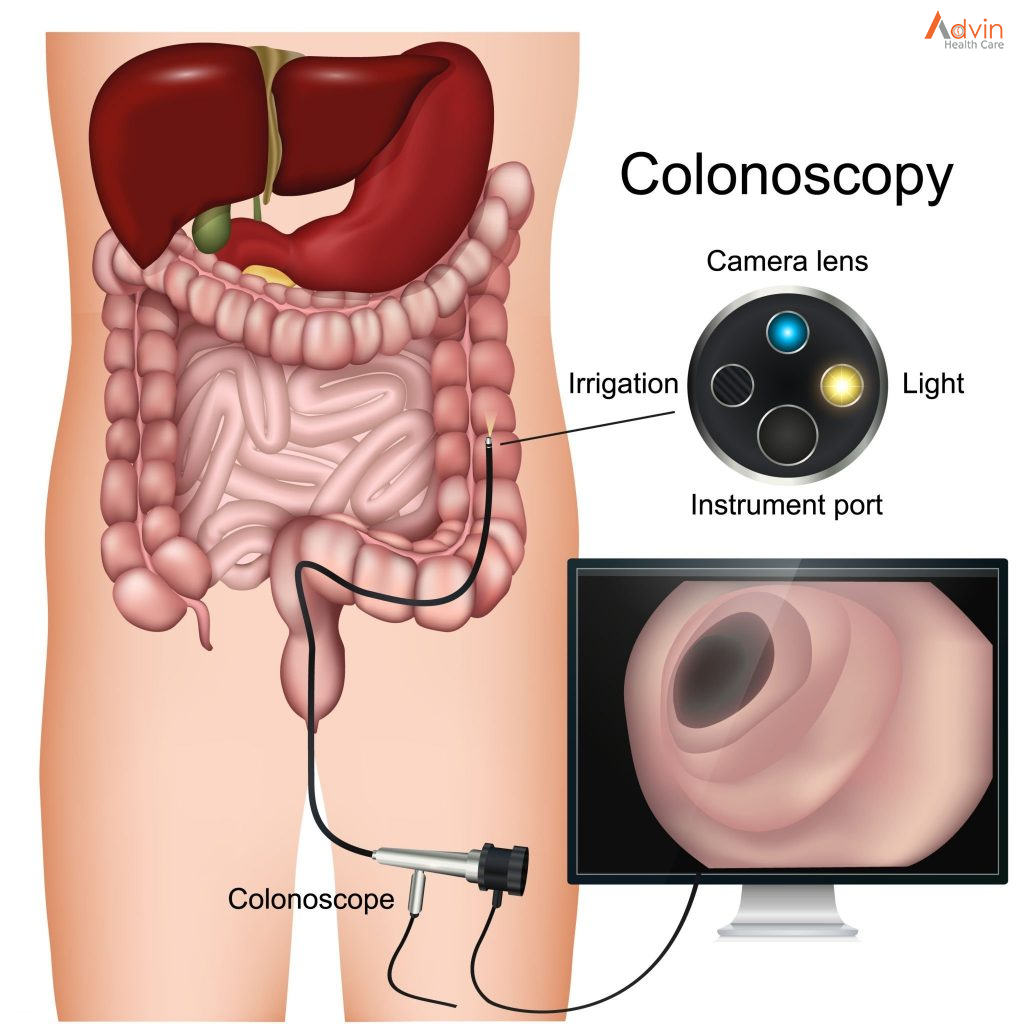
- Laparoscope
- Laparoscopic Grasper
- Bipolar Grasper
- Clip Applicator
- Hem ‘O’ Lock Applicator
- Veress needle
- Endo loop
- Endo Bag
- Electrosurgical Unit
- Co2 insufflator
- Led light Source
- Endoscopy Camera system
- Monopolar L Hooks