Prostatectomy Surgery
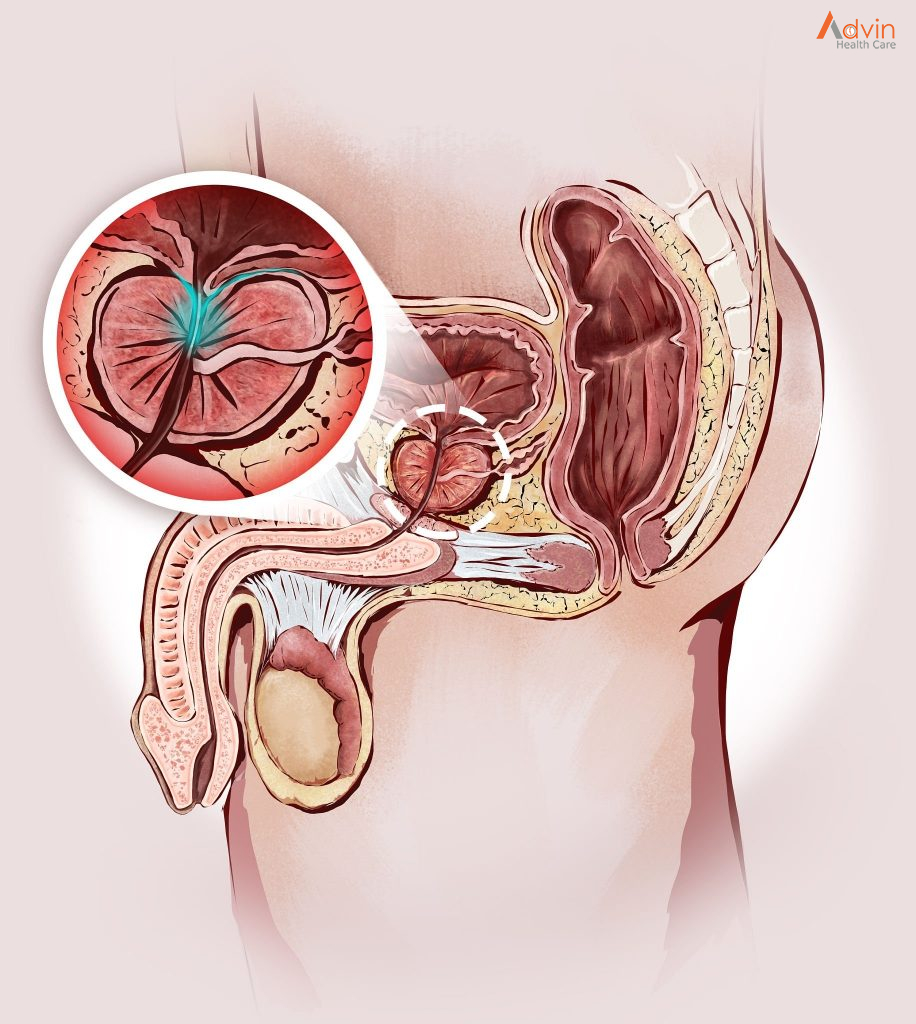
Prostatectomy is surgery to remove part or all of the prostate gland. The prostate gland is situated in the male pelvis, below the urinary bladder. It surrounds the urethra, which carries urine from the bladder to the penis.
The procedure is used to treat a number of conditions affecting the prostate. It’s most commonly used as a treatment for prostate cancer.
Prostatectomy can be performed in several ways, depending on the condition involved. Options include minimally invasive surgery performed with robotic assistance and traditional open surgery.
A common surgical approach to prostatectomy includes making a surgical incision and removing the prostate gland (or part of it). This may be accomplished with either of two methods, the retropubic or suprapubic incision (lower abdomen), or a perineum incision (through the skin between the scrotum and the rectum).
What is the prostate gland?
The prostate gland is about the size of a walnut and surrounds the neck of a man’s bladder and urethra—the tube that carries urine from the bladder. It’s partly muscular and partly glandular, with ducts opening into the prostatic portion of the urethra. It’s made up of three lobes, a center lobe with one lobe on each side.
As part of the male reproductive system, the prostate gland’s primary function is to secrete a slightly alkaline fluid that forms part of the seminal fluid (semen), a fluid that carries sperm. During male climax (orgasm), the muscular glands of the prostate help to propel the prostate fluid, in addition to sperm that was produced in the testicles, into the urethra. The semen then travels through the tip of the penis during ejaculation.
Researchers don’t know all the functions of the prostate gland. However, the prostate gland plays an important role in both sexual and urinary function. It’s common for the prostate gland to become enlarged as a man ages, and it’s also likely for a man to encounter some type of prostate problem in his lifetime.
Many common problems that don’t require a radical prostatectomy are associated with the prostate gland. These problems may occur in men of all ages and include:
- Benign prostatic hyperplasia (BPH) . This is an age-related enlargement of the prostate that isn’t malignant. BPH is the most common noncancerous prostate problem, occurring in most men by the time they reach their 60s. Symptoms are slow, interrupted, or weak urinary stream; urgency with leaking or dribbling; and frequent urination, especially at night. Although it isn’t cancer, BPH symptoms are often similar to those of prostate cancer.
- Prostatism. This involves decreased urinary force due to obstruction of flow through the prostate gland. The most common cause of prostatism is BPH.
- Prostatitis. Prostatitis is inflammation or infection of the prostate gland characterized by discomfort, pain, frequent or infrequent urination, and, sometimes, fever.
- Prostatalgia. This involves pain in the prostate gland, also called prostatodynia. It’s frequently a symptom of prostatitis.
There are different ways to achieve the goal of removing the prostate gland when there’s cancer. Methods of performing prostatectomy include:
- Surgical removal includes a radical prostatectomy (RP), with either a retropubic or perineal approach. Radical prostatectomy is the removal of the entire prostate gland. Nerve-sparing surgical removal is important to preserve as much function as possible.
- Transurethral resection of the prostate, or TURP, which also involves removal of part of the prostate gland, is an approach performed through the penis with an endoscope (small, flexible tube with a light and a lens on the end). This procedure doesn’t cure prostate cancer but can remove the obstruction while the doctors plan for definitive treatment.
- Laparoscopic surgery, done manually or by robot, is another method of removal of the prostate gland.
Are there different types of radical prostatectomy?
There are several methods of radical prostatectomy:
- Radical prostatectomy with retropubic (suprapubic) approach. This is the most common surgical approach used by urologists (doctors who specialize in diseases and surgery of the urinary tract). If there’s reason to believe the cancer has spread to the lymph nodes, the doctor will remove lymph nodes from around the prostate gland, in addition to the prostate gland. Cancer has spread beyond the prostate gland if it’s found in the lymph nodes. If that’s the case, then surgery may be discontinued, since it won’t treat the cancer adequately. In this situation, additional treatments may be used.
- Nerve-sparing prostatectomy approach. If the cancer is tangled with the nerves, it may not be possible to maintain the nerve function or structure. Sometimes nerves must be cut in order to remove the cancerous tissue. If both sides of the nerves are cut or removed, the man will be unable to have an erection. This won’t improve over time (although there are interventions that may restore erectile function).If only one side of the bundle of nerves is cut or removed, the man may have less erectile function, but will possibly have some function left. If neither nerve bundle is disturbed during surgery, function may remain normal. However, it sometimes takes months after surgery to know whether a full recovery will occur. This is because the nerves are handled during surgery and may not function properly for a while after the procedure.
- Laparoscopic radical prostatectomy. The surgeon makes several small cuts and long, thin tools are placed inside the cuts. The surgeon puts a thin tube with a video camera (laparoscope) inside one of the cuts and instruments through others. This helps the surgeon see inside during the procedure.
- Robotic-assisted laparoscopic prostatectomy . Sometimes laparoscopic surgery is done using a robotic system. The surgeon moves the robotic arm while sitting at a computer monitor near the operating table. This procedure requires special equipment and training. Not every hospital can do robotic surgery.
- Radical prostatectomy with perineal approach. Radical perineal prostatectomy is used less frequently than the retropubic approach. This is because the nerves can’t be spared as easily, nor can lymph nodes be removed by using this surgical technique. However, this procedure takes less time and may be an option if the nerve-sparing approach isn’t needed. This approach is also appropriate if lymph node removal isn’t required. Perineal prostatectomy may be used if other medical conditions rule out using a retropubic approach.With the retropubic approach, there is a smaller, hidden incision for an improved cosmetic effect. Also, major muscle groups are avoided. Therefore, there’s generally less pain and recovery time.
What you can expect
Before the procedure
Prostatectomy is usually done using general anesthesia, which means you’re not awake during the procedure. Your doctor may also give you an antibiotic right before surgery to help prevent infection.
During the procedure
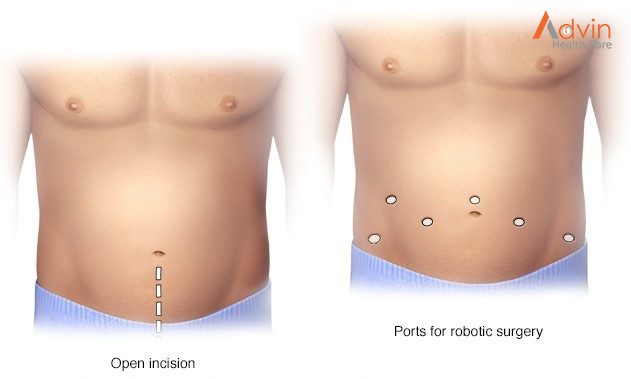
- Robot-assisted radical prostatectomy.Your surgeon sits at a remote-control console a short distance from you and the operating table and precisely controls the motion of the surgical instruments using two hand-and-finger control devices. The console displays a magnified, 3D view of the surgical area that enables the surgeon to visualize the procedure in much greater detail than in traditional laparoscopic surgery. The robotic system allows smaller and more-precise incisions, which for some men promotes faster recovery than traditional open surgery does. Just as with open retropubic surgery, the robotic approach enables nerve-sparing techniques that may preserve both sexual potency and continence in the appropriately selected person.
- Open radical prostatectomy.Your surgeon makes an incision in your lower abdomen, from below your navel to just above your pubic bone. After carefully dissecting the prostate gland from surrounding nerves and blood vessels, the surgeon removes the prostate along with nearby tissue. The incision is then closed with sutures.
- Simple prostatectomy.At the start of the procedure, your doctor may insert a long, flexible viewing scope (cystoscope) through the tip of your penis to see inside the urethra, bladder and prostate area. Your doctor will then insert a tube (Foley catheter) into the tip of your penis that extends into your bladder to drain urine during the procedure. The location of incisions will depend on what technique your doctor uses. If you also have a hernia or bladder problem, your doctor may use the surgery as an opportunity to repair it. Once your doctor has removed the part of your prostate causing symptoms, one to two temporary drain tubes may be inserted through punctures in your skin near the surgery site. One tube goes directly into your bladder (suprapubic tube), and the other tube goes into the area where the prostate was removed (pelvic drain).
After the procedure
- You’ll be given IV pain medications.Your doctor may give you prescription pain pills to take after the IV is removed.
- Your doctor will have you walk the day of or the day after surgery.You’ll also do exercises to move your feet while you’re in bed.
- You’ll likely go home the day after surgery.When your doctor thinks it’s safe for you to go home, the pelvic drain is taken out. You may need to return to the doctor in one or two weeks to have staples taken out.
- You’ll return home with a catheter in place.Most men need a urinary catheter for seven to 10 days after surgery. Full recovery of urinary control can take up to a year after surgery.
Make sure you understand the post-surgery steps you need to take, and any restrictions such as driving or lifting heavy things:
- You’ll need to resume your activity level gradually.You should be back to your normal routine in about four to six weeks.
- You’ll need to see your doctor a few times to make sure everything is OK. Most men see their doctors after about six weeks and then again every three months for the first year, and twice in the second year after surgery. If you have any problems or concerns, you may need to see your doctor sooner or more often.
- You’ll probably be able to resume sexual activity after recuperating from surgery.After simple prostatectomy, you can still have an orgasm during sex, but you’ll ejaculate very little or no semen. After radical prostatectomy, full recovery of erectile function may take as long as 18 months for some men.
Advin Prostatectomy Surgery
- Stainless Steel Bowl
- Sterilizing Stainless Steel Box
- Reverdin needle
- Metzembaun Scissors Curved
- Operating Scissors
- Farabeuf Retractor
- Judd‐Masson Retractor with median blade
- Malleable Blade Retractor
- Kocher Forceps
- Rochester‐Pean Forceps Curved
- Mair Polypus Forceps Straight
- Allis Tissue Forceps
- Backhaus Towel Forceps
- Chaput Forceps
- J.L Faure Forceps Curved
- Leriche Forceps Straight
- Museux Forceps Straight
- Murphy‐pean forceps straight
- Tissue Forceps
- Dissecting Forceps No Teeth
- Heart Shaped Forceps
- Stratte Needle Holder
- Probe With Tread

