ACL reconstruction is surgery to replace a torn anterior cruciate (KROO-she-ate) ligament (ACL) — a major ligament in your knee. ACL injuries most commonly occur during sports that involve sudden stops and changes in direction — such as soccer, football, basketball and volleyball.
Ligaments are strong bands of tissue that attach one bone to another bone. During ACL reconstruction, the torn ligament is removed and replaced with a band of tissue that usually connects muscle to bone (tendon). The graft tendon is taken from another part of your knee or from a deceased donor.
ACL reconstruction is an outpatient surgery that’s performed by a doctor who specializes in surgical procedures of the bones and joints (orthopedic surgeon).
Why it’s done
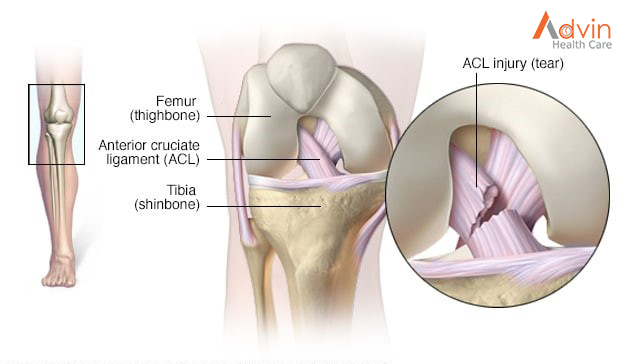
The ACL — one of two ligaments that crosses the middle of the knee — connects your thighbone to your shinbone and helps stabilize your knee joint.
Most ACL injuries happen during sports and fitness activities that can put stress on the knee:
- Suddenly slowing down and changing direction (cutting)
- Pivoting with your foot firmly planted
- Landing from a jump incorrectly
- Stopping suddenly
- Receiving a direct blow to the knee
A course of physical therapy may successfully treat an ACL injury for people who are relatively inactive, engage in moderate exercise and recreational activities, or play sports that put less stress on the knees.
ACL reconstruction is generally recommended if:
- You’re an athlete and want to continue in your sport, especially if the sport involves jumping, cutting or pivoting
- More than one ligament is injured
- You have a torn meniscus that requires repair
- The injury is causing your knee to buckle during everyday activities
- You’re young (though other factors, such as activity level and knee instability, are more important than age)
What Is ACL Surgery?

ACL surgery is a procedure that doctors use to replace a torn ligament in your knee.
The ACL (anterior cruciate ligament) is a band of tissue inside your knee. It gets damaged when it stretches or tears. ACL injuries are common among people who play sports because they make movements that can put a lot of stress on the knee, like:
- Changing direction quickly (cutting)
- Stopping suddenly
- Planting your foot and pivoting
- Landing wrong after a jump
When your ACL is healthy, it helps to hold together the bones of your knee. It also helps to keep your knee stable. If it gets damaged, you may have trouble putting pressure on your knee, walking, or playing sports.
If you strain or slightly tear your ACL, it may heal over time with your doctor’s help and physical therapy. But if it’s completely torn, you may need to have it replaced — especially if you’re young and active or an athlete who wants to keep playing sports. If you’re older or less active, your doctor might recommend treatments that don’t require surgery.
Types of ACL Surgery
When your doctor removes your torn ACL, they put a tendon in its place. (Tendons connect muscle to bone.) The goal is to get your knee stable again and give it the full range of motion it had before you got hurt.
When the tendon is put into your knee, it’s known as a graft. Three types of grafts can be used with ACL surgery:
- Autograft. Your doctor uses a tendon from somewhere else in your body (like your other knee, hamstring, or thigh).
- Allograft. This type of graft uses tissue from someone else (a deceased donor).
- Synthetic graft. This is when artificial materials replace the tendon. Silver fibers and silk were among the first ones used (in the early part of the 20th century). More advanced options are available now, like carbon fiber and Teflon, but researchers are still working to find the best material for ACL replacement.
ACL Surgery Procedure
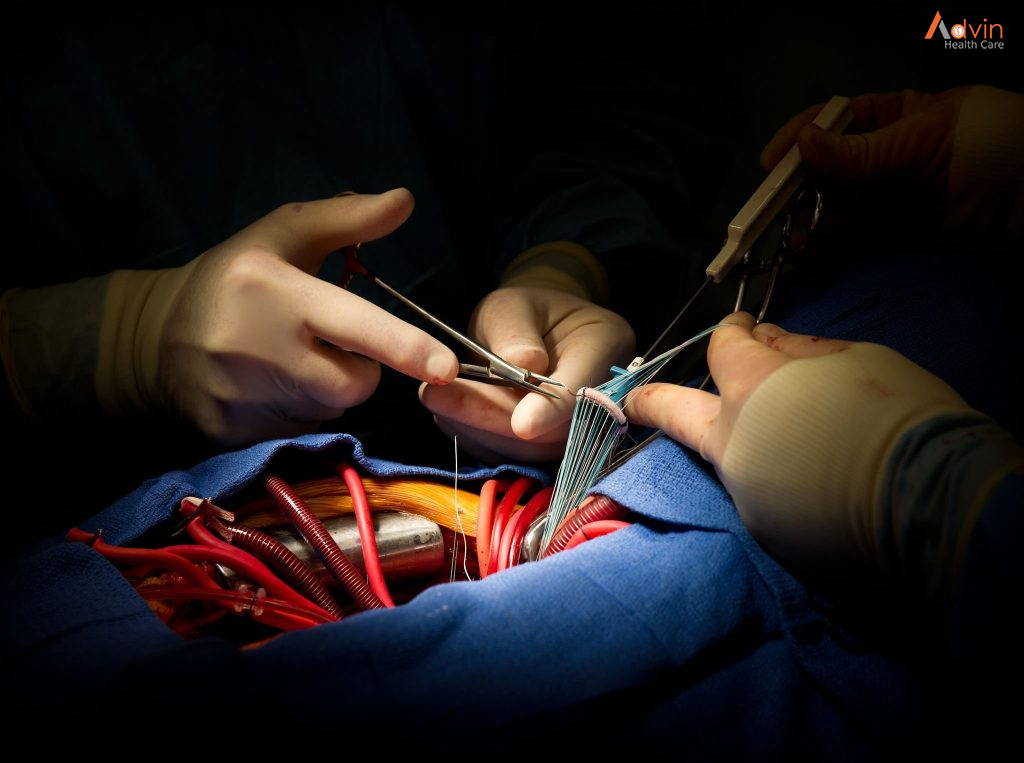
Doctors typically use arthroscopic surgery on your ACL. This means they insert tiny tools and a camera through small cuts around your knee. This method causes less scarring of the skin than open-knee surgery does.
The procedure takes about an hour. You may have general anesthesia, which puts you to sleep through the surgery, or you may have regional anesthesia, when your doctor puts medicine in your back so you won’t feel anything in your legs for a few hours. If you have regional anesthesia, you probably will also get medicine that helps you relax during the procedure.
The first step is to place the graft at the right spot. Then, your doctor will drill two holes, called “tunnels.” They’ll put one in the bone above your knee and another in the bone below it. They’ll place screws in the tunnels to hold the graft in place. It serves as a sort of bridge that a new ligament will grow on as you heal. It can take months for a new ACL to grow in fully.
After surgery, most people are able to go home the same day. Your doctor will have you stay off your leg, rest your knee, and wear a brace to protect the joint.
Doctors are also involved in research to see if a new type of ACL surgery is better than the standard care. It’s called bridge-enhanced ACL repair (BEAR).