Blood Donation
Blood donation is a vital part of worldwide healthcare. It relates to blood transfusion as a life-sustaining and life-saving procedure as well as a form of therapeutic phlebotomy as a primary medical intervention. Over one hundred million units of blood are donated each year throughout the world. This article will concisely discuss a short history of blood donation origin and purpose, blood testing, donor eligibility and selection, adverse effects of donation, blood donation as a primary medical intervention, and a brief discussion of pathogen reduction and inactivation for donated blood.
Blood donation is most often performed by inserting a large bore needle (16G or 18G) into a peripheral vein, usually within the antecubital fossa. Veins on the dorsum of the hand or other prominent veins may be used in some individuals who do not have an otherwise easily accessible antecubital vein.
Blood donation is a procedure wherein a person donates his blood to save a fellow human. The blood is then adequately stored in the blood bank and used to transfuse whenever necessary.
Blood Typing
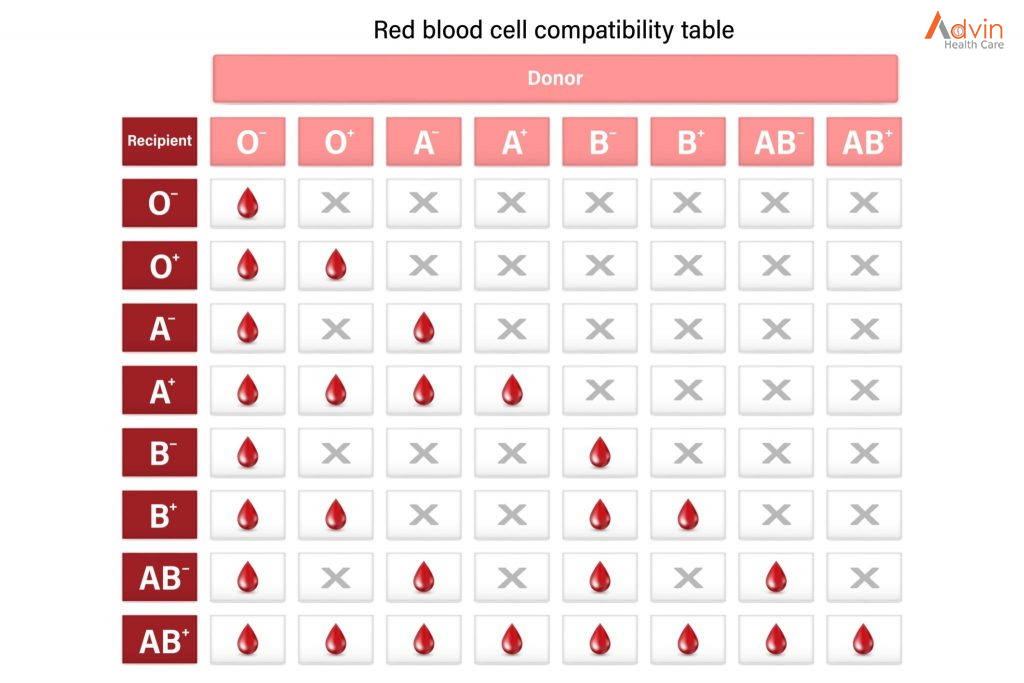
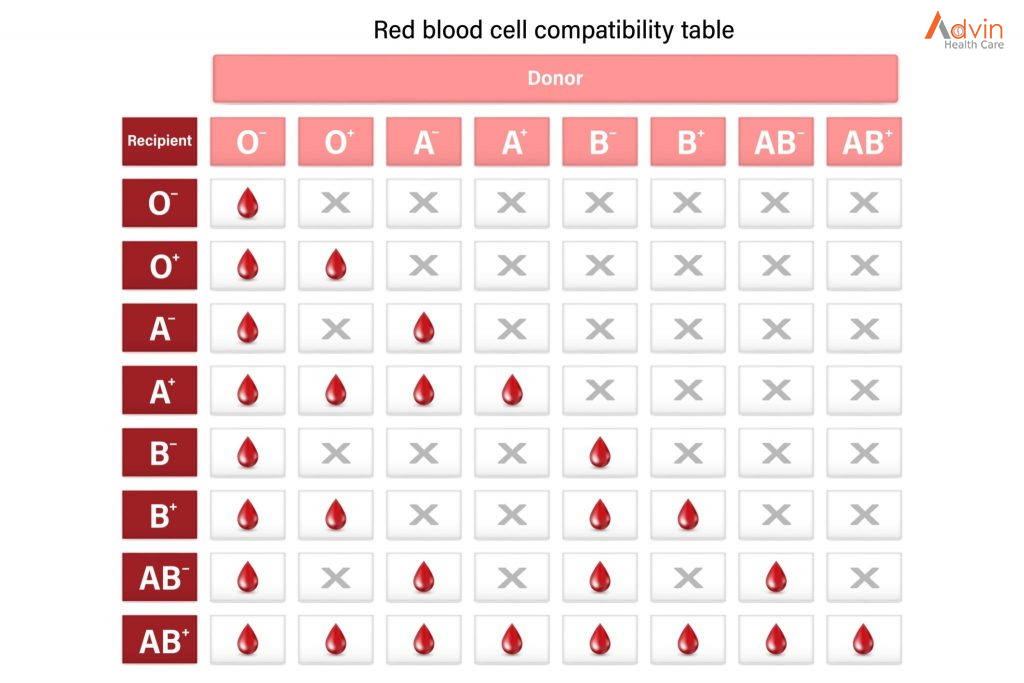
People have different blood types. Blood type is determined by whether certain antigens (complex sugar or protein molecules that can trigger an immune response) are present on the surface of red blood cells. Blood cell antigens include blood group antigens A and B and Rh factor.
The four main blood types are A, B, AB, and O (distribution in general population)
- A: Antigen A (but not B) is present. (40%)
- B: Antigen B (but not A) is present. (10%)
- AB: Antigens A and B are present. (5%)
- O: Neither antigen A nor B is present. (45%)
Also, blood may be Rh-positive (Rh factor is present on the surface of the red blood cells, 85% of people) or Rh-negative (Rh factor is absent, 15% of people).
Normally, if people lack an A and/or a B antigen, they have naturally occurred antibodies against the antigen or antigens that they lack. For example, people with blood type A have naturally occurring anti-B antibody, and people with blood type O (who lack both A and B antigens) have naturally occurring anti-A and anti-B antibodies. In addition to A and B antigens, there are several other blood group antigens also present on red blood cells. However, people do not have naturally occurring antibodies against these antigens. Such antibodies develop only if people are exposed to these antigens by transfusion.
Blood Transfusion
Transfusion medicine is a specialized branch of hematology that is concerned with the study of blood groups, along with the work of a blood bank to provide a transfusion service for blood and other blood products. Across the world, blood products must be prescribed by a medical doctor (licensed physician or surgeon) in a similar way as medicines.
Much of the routine work of a blood bank involves testing blood from both donors and recipients to ensure that every individual recipient is given blood that is compatible and is as safe as possible. If a unit of incompatible blood is transfused between a donor and recipient, a severe acute hemolytic reaction with hemolysis (RBC destruction), kidney failure and shock is likely to occur, and death is a possibility. Antibodies can be highly active and can attack RBCs and bind components of the complement system to cause massive hemolysis of the transfused blood.
Patients should ideally receive their own blood or type-specific blood products to minimize the chance of a transfusion reaction. It is also possible to use the patient’s own blood for transfusion. This is called autologous blood transfusion, which is always compatible with the patient. The procedure of washing a patient’s own red blood cells goes as follows: The patient’s lost blood is collected and washed with a saline solution. The washing procedure yields concentrated washed red blood cells. The last step is reinfusing the packed red blood cells into the patient. There are multiple ways to wash red blood cells. The two main ways are centrifugation and filtration methods. This procedure can be performed with microfiltration devices like the Hemoclear filter. Risks can be further reduced by cross-matching blood, but this may be skipped when blood is required for an emergency. Cross-matching involves mixing a sample of the recipient’s serum with a sample of the donor’s red blood cells and checking if the mixture agglutinates, or forms clumps. If agglutination is not obvious by direct vision, blood bank technologist usually check for agglutination with a microscope. If agglutination occurs, that particular donor’s blood cannot be transfused to that particular recipient. In a blood bank it is vital that all blood specimens are correctly identified, so labelling has been standardized using a barcode system known as ISBT 128.
The blood group may be included on identification tags or on tattoos worn by military personnel, in case they should need an emergency blood transfusion. Frontline German Waffen-SS had blood group tattoos during World War II.
Rare blood types can cause supply problems for blood banks and hospitals. For example, Duffy-negative blood occurs much more frequently in people of African origin, and the rarity of this blood type in the rest of the population can result in a shortage of Duffy-negative blood for these patients. Similarly, for RhD negative people there is a risk associated with travelling to parts of the world where supplies of RhD negative blood are rare, particularly East Asia, where blood services may endeavor to encourage Westerners to donate blood.
Who is a suitable candidate for blood donation?

Blood donation is a noble cause. Though most of us may want to do it, not everybody is eligible. In India, a blood donor must be at least 18 years of age, in good health and at ideal weight.
The hospital staff takes a sample of your blood to check for your eligibility. They evaluate the amount of haemoglobin in the blood, and if the levels are low, you may not be allowed for blood donation.
The hospital will also ask you various questions to map your medical history. These are targeted to understand if you have higher chances of carrying bloodborne infections.
The following situations may bar a person from donating blood:
- Consuming drugs or steroids in the past three months
- A person suffering from congenitalcoagulation deficiency
- Testing positive for HIV
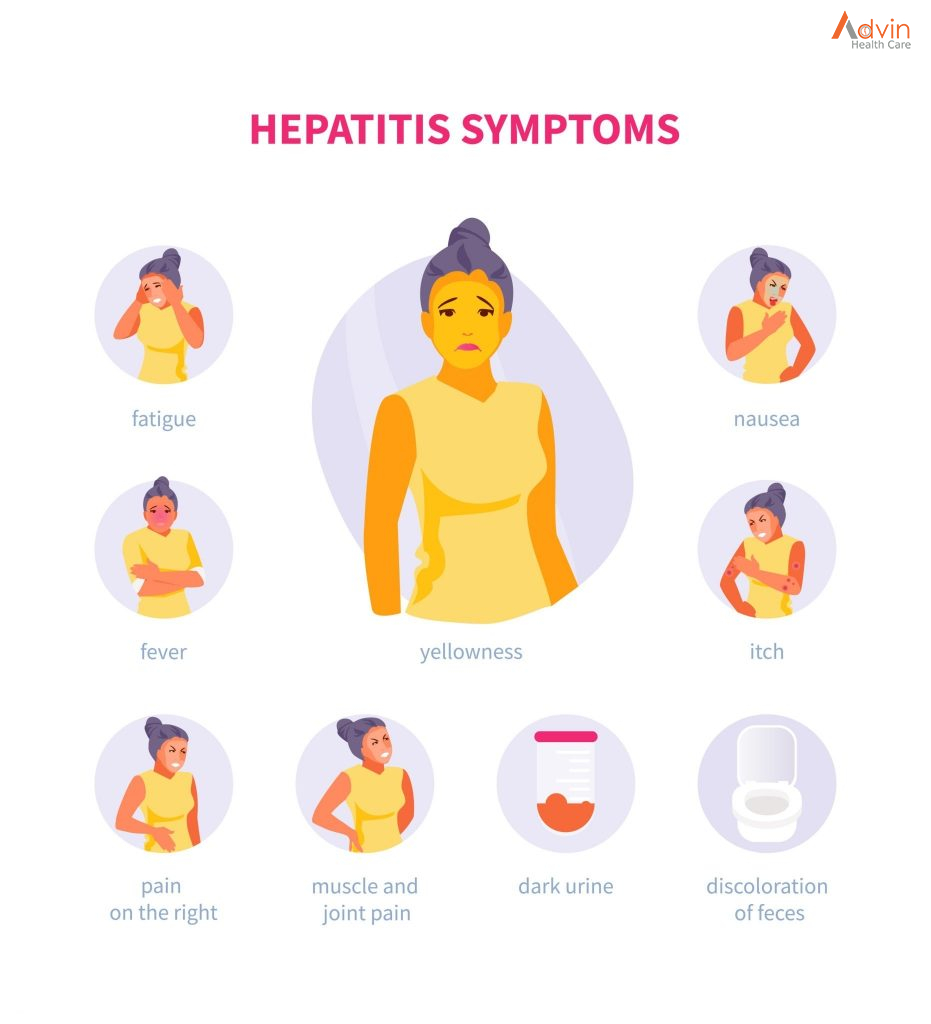
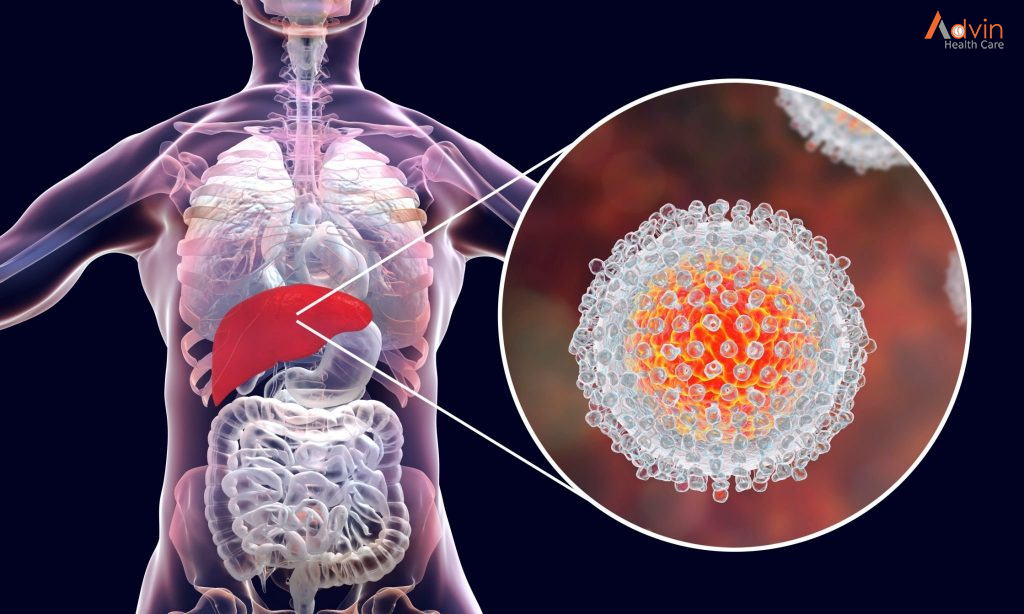
- In a sexual relationship with a person suffering from viral hepatitis
- A history of babesiosis
Why Is Blood Donation Conducted?
Blood plays a crucial role in our body. It is responsible for all the other functions in the body that keep us alive. However, some situations lead to a lack of blood, and when the same is not transfused into the body within the stipulated time, the person may lose his life.
Deaths due to blood loss during accidents, calamities, pregnancy, childbirth, major surgery, and severe anemia are avoidable deaths. In all these situations, the availability of blood could save lives. As considerate humans, we must realize that preventable deaths are the worst, and blood donation can help cope with this situation.
What Are the Different Kinds of Blood Donation?

Voluntary blood donation is of four types. These include whole blood, plasma, red blood cells, and platelet donations.
The whole blood donation procedure is the most common one you can witness. People with all blood groups are eligible for this procedure, wherein half a liter of blood is taken. The blood is either transfused as a whole or separated into red blood cells, platelets, and plasma.
Platelets are tiny cells in your body—these help to stop bleeding by clotting the blood. People with clotting problems, cancer, organ transplants, and major surgeries may need platelets. Once donated, platelets have to be used within five days.
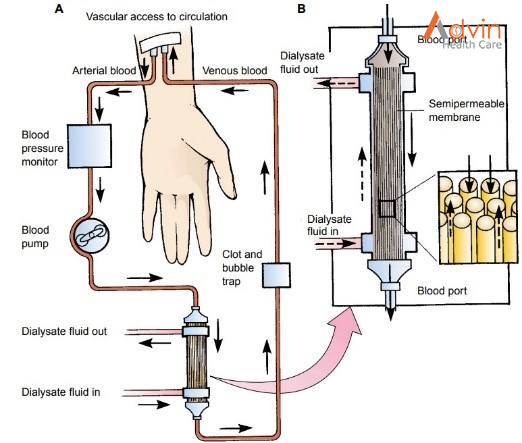
An apheresis machine collects your platelets with some plasma: the red blood cells and most of the plasma return to your body.
People suffering from liver conditions, severe bacterial infections, or burns require plasma donations. These conditions need plasma for clotting the blood and stopping bleeding. Like platelet donation, plasma is also taken through the apheresis machine, and the other blood components are returned to the donor.
Plasma from the AB blood group is high in demand as it can be transfused to any person regardless of the blood group. One can donate plasma every 28 days.
Red blood cells play a crucial role in carrying oxygen to every part of the body and hence are highly vital. Patients who lose a major chunk of their blood through excessive trauma, major surgery, or acute anemia may require blood donation from red blood cells.
Here too, red blood cells are extracted from the blood through the apheresis machine while the rest is returned to the donor. Your body will require significant time to replace red blood cells. Hence, doctors advise you to maintain a gap of 168 days before your next blood donation.
If you think of opting for any of the above blood donation types, meet a doctor for expert advice.
Are There Any Benefits of Blood Donation?
The most significant benefit of donating blood is that you get to save lives. People stuck in disasters, calamities, and fatal diseases can live longer with blood transfusion. For many, it can help to prevent deaths from fatal accidents and trauma.
While you will be helping people, there are also multiple benefits to your own body. Blood donation is healthy for the donor. Regular blood donation offers the following benefits.
- Better emotional wellbeing
Blood donation helps you think positively about life. It is an act that can save a stranger’s life, making you feel worthwhile.
- Improvement in cholesterol levels
Though the reason for the same is yet to be unearthed, donating blood does make way for good cholesterol.
For some people, high iron levels can be a cause of worry. Donating blood can reverse the condition by removing red blood cells, consequently lowering the iron levels.
Recipient safety
Donors are screened for health risks that could make the donation unsafe for the recipient. Some of these restrictions are controversial, such as restricting donations from men who have sex with men (MSM) because of the risk of transmitting HIV. In 2011, the UK (excluding Northern Ireland) reduced its blanket ban on MSM donors to a narrower restriction which only prevents MSM from donating blood if they have had sex with other men within the past year.[ A similar change was made in the US in late 2015 by the FDA. In 2017, the UK and US further reduced their restrictions to three months. Autologous donors are not always screened for recipient safety problems since the donor is the only person who will receive the blood. Since the donated blood may be given to pregnant women or women of child-bearing age, donors taking teratogenic (birth defect-causing) medications are deferred. These medications include acitretin, etretinate, isotretinoin, finasteride, and dutasteride.
Donors are examined for signs and symptoms of diseases that can be transmitted in a blood transfusion, such as HIV, malaria, and viral hepatitis. Screening may include questions about risk factors for various diseases, such as travel to countries at risk for malaria or variant Creutzfeldt–Jakob disease (vCJD). These questions vary from country to country. For example, while blood centers in Québec and the rest of Canada, Poland, and many other places defer donors who lived in the United Kingdom for risk of vCJD, donors in the United Kingdom are only restricted for vCJD risk if they have had a blood transfusion in the United Kingdom.
Donor safety

The donor is also examined and asked specific questions about their medical history to make sure that donating blood is not hazardous to their health. The donor’s hematocrit or hemoglobin level is tested to make sure that the loss of blood will not make them anemic, and this check is the most common reason that a donor is ineligible. Accepted hemoglobin levels for blood donations, by the American Red Cross, is 12.5g/dL (for females) and 13.0g/dL (for males) to 20.0g/dL, anyone with a higher or lower hemoglobin level cannot donate. Pulse, blood pressure, and body temperature are also evaluated. Elderly donors are sometimes also deferred on age alone because of health concerns. In addition to age, weight and height are important factors when considering the eligibility for donors. For example, the American Red Cross requires a donor to be 110 pounds (50 kg) or more for whole blood and platelet donation and at least 130 pounds (59 kg) (males) and at least 150 pounds (68 kg) (females) for power red donations (double red erythrocytapheresis). The safety of donating blood during pregnancy has not been studied thoroughly, and pregnant women are usually deferred until six weeks after the pregnancy.