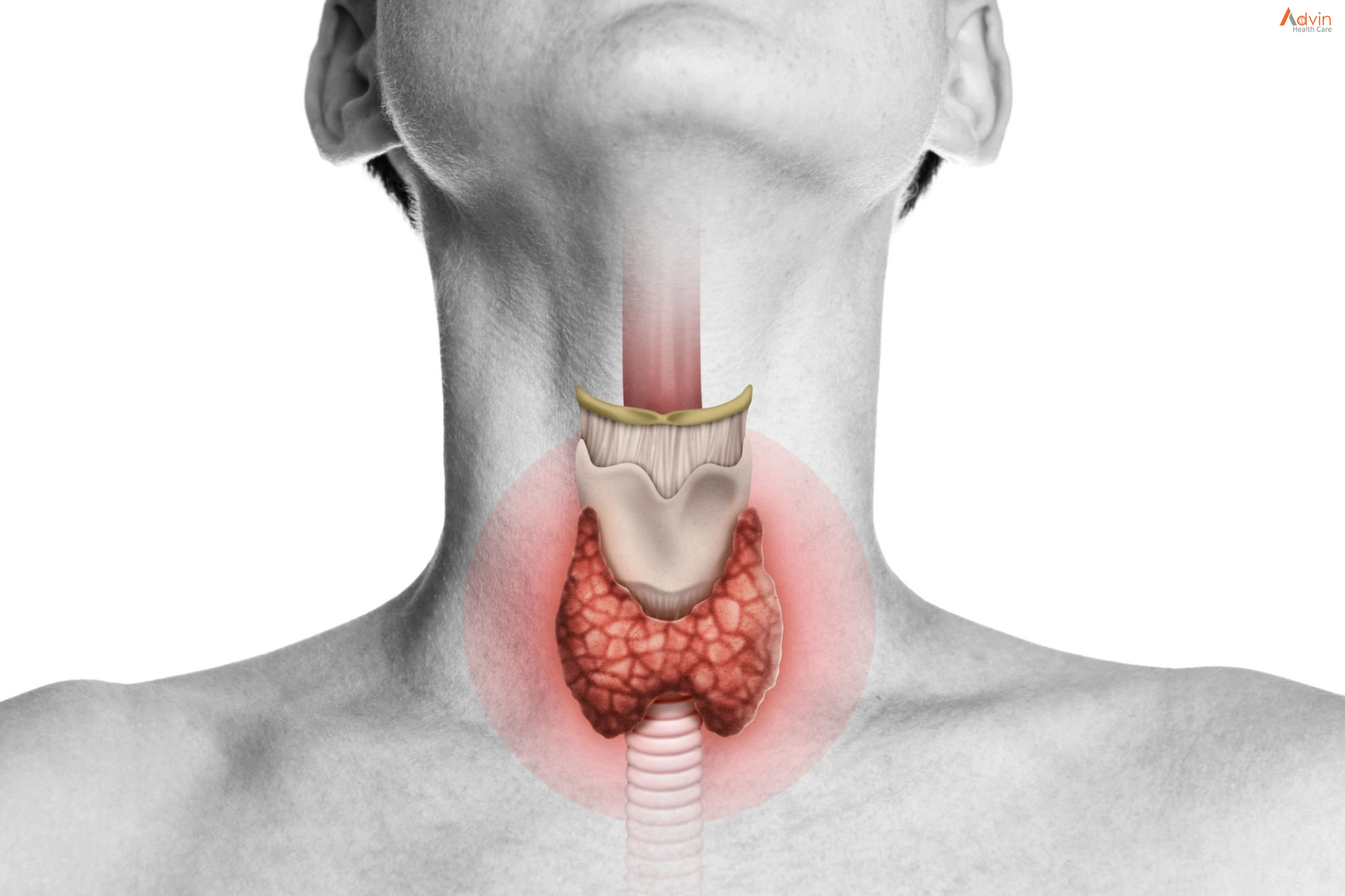
Thyroidectomy is the surgical removal of all or part of your thyroid gland. Your thyroid is a butterfly-shaped gland located in the front of your neck. It makes hormones that control every part of your metabolism, from your heart rate to how quickly you burn calories.
Health care providers perform thyroidectomy to treat thyroid disorders. These include cancer, noncancerous enlargement of the thyroid (goiter) and overactive thyroid (hyperthyroidism).
How much of your thyroid gland is removed during thyroidectomy depends on the reason for the surgery. If you need only part of your thyroid removed (partial thyroidectomy), your thyroid may work normally after surgery. If you need your entire thyroid removed (total thyroidectomy), you need daily treatment with thyroid hormone to replace your thyroid’s natural function.
What is a thyroidectomy?
A thyroidectomy is the surgical removal of all (total thyroidectomy) or part (partial thyroidectomy) of your thyroid gland — the butterfly-shaped organ in your neck.
Thyroidectomy is the main surgical treatment for thyroid cancer and is a treatment option for certain thyroid conditions, including:
- Thyroid nodules: A thyroid nodule is a growth (lump) of thyroid cells in your thyroid gland. Thyroid nodules are usually benign (noncancerous), but they can be malignant (cancerous). Sometimes, thyroid nodules can produce excess thyroid hormone, which causes certain symptoms.
- Goiter: Goiter is an enlarged thyroid gland with or without thyroid nodules. If it grows large enough, it can put pressure on your trachea or food pipe (esophagus) and make it more difficult to breathe and swallow.
- Hyperthyroidism: Hyperthyroidism (overactive thyroid) is a condition in which your thyroid creates and releases more hormones than you need. It has several causes, and surgery is one of the treatment options for the condition.
Why it’s done

Your doctor may recommend thyroidectomy if you have conditions such as:
- Thyroid cancer. Cancer is the most common reason for thyroidectomy. If you have thyroid cancer, removing most or all of your thyroid will likely be a treatment option.
- Noncancerous enlargement of the thyroid (goiter). Removing all or part of your thyroid gland may be an option for a large goiter. A large goiter may be uncomfortable or make it hard to breathe or swallow. A goiter may also be removed if it’s causing your thyroid to be overactive.
- Overactive thyroid (hyperthyroidism). In hyperthyroidism, your thyroid gland produces too much of the hormone thyroxine. Thyroidectomy may be an option if you have problems with anti-thyroid drugs, or if you don’t want radioactive iodine therapy. These are two other common treatments for hyperthyroidism.
- Suspicious thyroid nodules. Some thyroid nodules can’t be identified as cancerous or noncancerous after testing a sample from a needle biopsy. If your nodules are at increased risk of being cancerous, you may be a candidate for thyroidectomy.
Types of Thyroid Operations

In general, there are three types of thyroid resections:
Total thyroidectomy: removal of the entire thyroid
A total thyroidectomy may be done for a variety of diseases including thyroid cancer, Graves’ disease (See Hyperthyroidism »), multinodular goiter, and substernal goiter, among others. In certain cases, the surgeon may choose to perform a near-total thyroidectomy in which a small piece of thyroid tissue is left behind usually in the area of the parathyroid glands and recurrent laryngeal nerve in order to avoid damaging these structures. After a total thyroidectomy, patients will need to take thyroid hormone replacement pills (one pill a day for the rest of their lives).
Thyroid lobectomy (aka hemithyroidectomy): removal of half of the thyroid
A thyroid lobectomy may be done for a variety of diseases including indeterminate lesions on fine needle biopsy (See Thyroid Nodules Diagnosis and Treatment »), a toxic nodule (See Hyperthyroidism »), substernal goiter, and an enlarging thyroid nodule, among others. In cases of indeterminate lesions, some surgeons refer to a thyroid lobectomy as a diagnostic lobectomy because the main purpose of the operation is to make a diagnosis – cancer or benign thyroid disease. The final pathology is ready approximately 1 week after the operation. Approximately 70% of patients who have half of a normal thyroid gland left in place will not require thyroid hormone replacement pills. This percent decreases in older women, patients with a personal or family history of Hashimoto’s thyroiditis or hypothyroidism, and patients with a family history of autoimmune disease.
Completion thyroidectomy: removal of any remaining thyroid tissue.
A completion thyroidectomy is usually done after a thyroid lobectomy reveals cancer in the first half of the thyroid but may also be done for multinodular goiter or hyperthyroidism. After a completion thyroidectomy, patients will need to take thyroid hormone replacement pills (one pill a day for the rest of their lives).
The decision as to which thyroid operation to perform depends on a number of factors including the type of disease and the patient’s preferences. It is critical to work with a team of thyroid specialists to choose the right operation for each individual patient.
Advin Thyroidectomy Instrument set
- Crile Wood Needle Holder Tungsten Carbide
- Allis Tissue Forceps
- Lahey Tenaculum Forceps
- Cushing Vein and Nerve Retractor
- Beckmann Dissector
- Senn-green
- Hemostatic Forceps Straight
- Metzenbaum Scissors Standard Curved
- Joseph Double Prong Skin Hook
- Joseph Skin Hook One
- Frazier Suction Tube
- Weitlaner Retractor
- Senn Miller Retractor
- Jansen Mastoid Retractor
- Iris Scissors Straight
- Webster Needle Holder
- Foerster Sponge Forceps Straight
- Backhaus Towel Clamp
- Gemini Mixter
- Crile Hemostatic Forceps Curved
- Kelly Hemostatic Forceps Curved
- Halstead Mosquito Forceps Curved
- Halstead Mosquito Forceps Straight
- Adson Tissue Forceps
- Adson Dressing Forceps
- Mayo Dissecting Scissors Straight
- Metzenbaum Dissecting Scissors Curved
- Iris Scissors Curved