Bariatric surgery is a term that refers to surgical procedures that assist in weight loss by making changes to the digestive system. The term “bariatric surgery” can be used to describe a variety of procedures, such as gastric bypass and other weight loss surgeries.
Gastric bypass and other weight-loss surgeries — known collectively as bariatric surgery —involve making changes to your digestive system to help you lose weight. Bariatric surgery is done when diet and exercise haven’t worked or when you have serious health problems because of your weight. Some procedures limit how much you can eat. Other procedures work by reducing the body’s ability to absorb nutrients. Some procedures do both.
While bariatric surgery can offer many benefits, all forms of weight-loss surgery are major procedures that can pose serious risks and side effects. Also, you must make permanent healthy changes to your diet and get regular exercise to help ensure the long-term success of bariatric surgery.
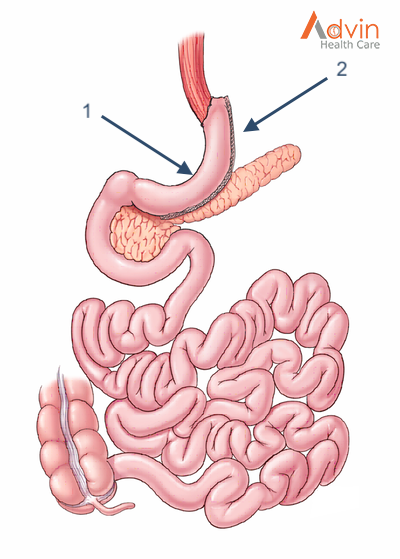
Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy, often called the “sleeve”, is performed by removing approximately 80% of the stomach. The remaining stomach is the size and shape of a banana.
The Procedure
- The stomach is freed from organs around it.
- Surgical staplers are used to remove 80% of the stomach, making it much smaller.
How it Works
The new stomach holds less food and liquid helping reduce the amount of food (and calories) that are consumed. By removing the portion of the stomach that produces most of the “hunger hormone”, the surgery has an effect on the metabolism. It decreases hunger, increases fullness, and allows the body to reach and maintain a healthy weight as well as blood sugar control. The simple nature of the operation makes it very safe without the potential complications from surgery on the small intestine.
Advantages
- Technically simple and shorter surgery time
- Can be performed in certain patients with high risk medical conditions
- May be performed as the first step for patients with severe obesity
- May be used as a bridge to gastric bypass or SADI-S procedures
- Effective weight loss and improvement of obesity related conditions
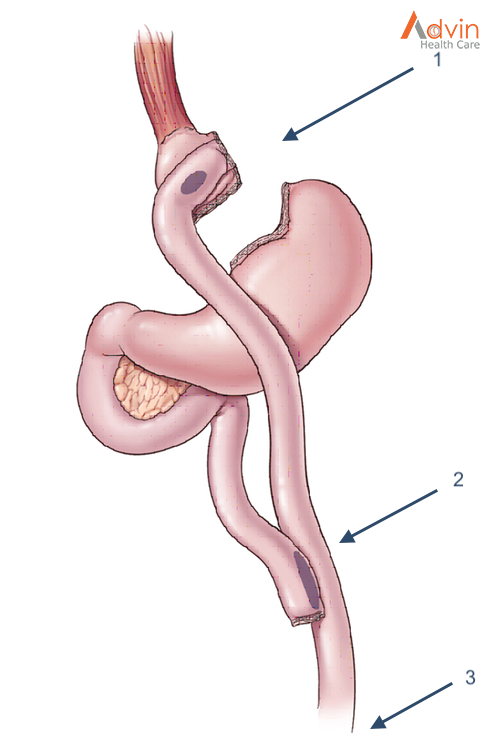
Roux-en-Y Gastric Bypass (RYGB)
The Roux-en-Y Gastric Bypass, often called the “gastric bypass”, has now been performed for more than 50 years and the laparoscopic approach has been refined since 1993. It is one of the most common operations and is very effective in treating obesity and obesity related diseases. The name is a French term meaning “in the form of a Y”.
The Procedure
- First, the stomach is divided into a smaller top portion (pouch) which is about the size of an egg. The larger part of the stomach is bypassed and no longer stores or digests food.
- The small intestine is also divided and connected to the new stomach pouch to allow food to pass. The small bowel segment which empties the bypassed or larger stomach is connected into the small bowel approximately 3-4 feet downstream, resulting in a bowel connection resembling the shape of the letter Y.
- Eventually the stomach acids and digestive enzymes from the bypassed stomach and first portion of the small intestine will mix with food that is eaten.
How it Works
The gastric bypass works in several ways. Like many bariatric procedures, the newly created stomach pouch is smaller and able to hold less food, which means fewer calories are ingested. Additionally, the food does not come into contact with the first portion of the small bowel and this results in decreased absorption. Most importantly, the modification of the food course through the gastrointestinal tract has a profound effect to decrease hunger, increase fullness, and allow the body to reach and maintain a healthy weight. The impact on hormones and metabolic health often results in improvement of adult onset diabetes even before any weight loss occurs. The operation also helps patients with reflux (heart burn) and often the symptoms quickly improve. Along with making appropriate food choices, patients must avoid tobacco products and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen.
Advantages
- Reliable and long-lasting weight loss
- Effective for remission of obesity-associated conditions
- Refined and standardized technique
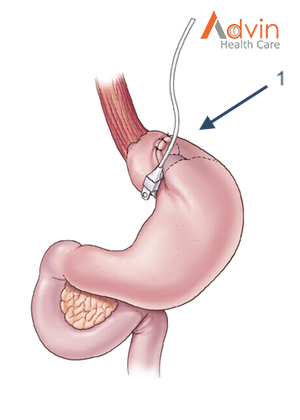
Adjustable Gastric Band (AGB)
The Adjustable Gastric Band is a device made of silicone that is placed around the top part of the stomach to limit the amount of food a person can eat. It has been available in the United States since 2001. The impact on obesity related diseases and long-term weight loss is less than with other procedures. Its use has therefore declined over the past decade.
The Procedure
- This device is placed and secured around the top part of the stomach creating a small pouch above the band.
How it Works
The feeling of fullness depends upon the size of the opening between the pouch and the rest of the stomach. The opening size can be adjusted with fluid injections through a port underneath the skin. Food goes through the stomach normally but is limited by the smaller opening of the band. It is less successful against type 2 diabetes and has modest effects on the metabolism.
Advantages
- Lowest rate of complications early after surgery
- No division of the stomach or intestines
- Patients can go home on the day of surgery
- The band can be removed if needed
- Has the lowest risk for vitamin and mineral deficiencies
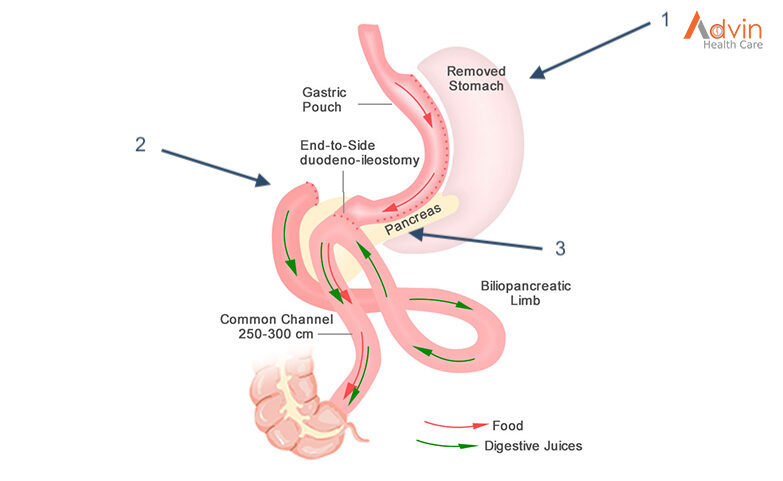
Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
The Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy, referred to as the SADI-S is the most recent procedure to be endorsed by the American Society for Metabolic and Bariatric Surgery. While similar to the BPD-DS, the SADI-S is simpler and takes less time to perform as there is only one surgical bowel connection.
The Procedure
- The operation starts the same way as the sleeve gastrectomy, making a smaller tube-shaped stomach.
- The first part of the small intestine is divided just after the stomach.
- A loop of intestine is measured several feet from its end and is then connected to the stomach. This is the only intestinal connection performed in this procedure.
How it Works
When the patient eats, food goes through the pouch and directly into the latter portion of the small intestine. The food then mixes with digestive juices from the first part of the small intestine. This allows enough absorption of vitamins and minerals to maintain healthy levels of nutrition. This surgery offers good weight loss along with less hunger, more fullness, blood sugar control and diabetes improvement.
Advantages
- Highly effective for long-term weight loss and remission of type 2 diabetes
- Simpler and faster to perform (one intestinal connection) than gastric bypass or BPD-DS
- Excellent option for a patient who already had a sleeve gastrectomy and is seeking further weight loss