Anterior cervical discectomy and fusion is a surgery to reduce or eliminate chronic pain in the neck and back due to a problem with the discs. Anterior cervical discectomy and fusion (ACDF) is an operation to remove a degenerative or herniated disc from the neck. After the surgeon removes the damaged disc, they fuse the bones together.
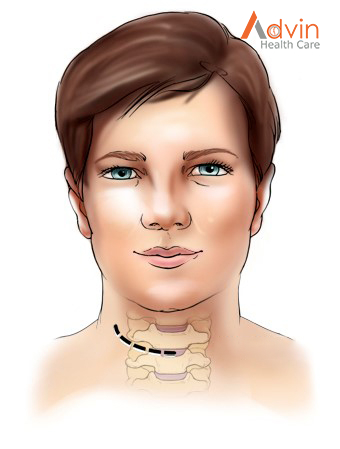
The surgery is anterior because the surgeon accesses the disc through the front of the neck, rather than through the back.
What is an anterior cervical discectomy & fusion?
Between each bone of the spinal column is a cushion called an invertebral disc. These discs prevent the bones from grinding against one another and act as shock absorbers during falls, exercise, and daily activities.
Sometimes these discs become damaged, causing pain that can range from moderate to intense. An ACDF procedure may be carried out on any of the discs in between the seven cervical bones.
It is easier for the surgeon to reach the spinal column through the throat because entering through the back of the neck can harm the neck muscles and spinal column. The surgeon then moves the tissue inside the neck and throat aside to access the spine and removes any damaged discs.
To ensure that the spine is aligned and to prevent the bones of the spine from rubbing against one another, the surgery typically includes fusion of at least two bones. It is at this point during the procedure that the surgeon replaces the disc.
There are a few options for disc replacement:
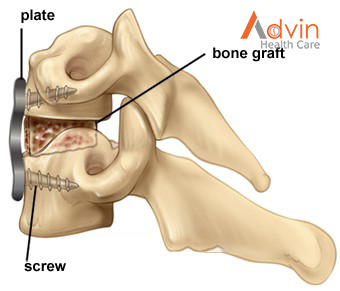
- Bone graft: A bone graft is when the surgeon attaches bone to the area to replace the disc. The bone may come from somewhere else in the person’s own body, or from a bone bank.
- Bone graft substitute: Similar to a bone graft, this approach uses human-manufactured materials that contain shavings from the person’s bones.
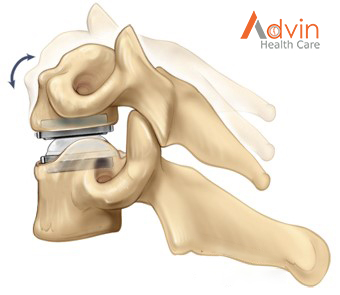
- Arthroplasty: This is when the surgeon replaces the disc with an artificial disc.
Once the replacement disc is in place, the surgeon uses a titanium plate and screws to attach the bones. When the surgery involves a bone graft, the bones will eventually grow together. Until that happens, the plate and screws provide stability.
An X-ray machine helps the surgeon ensure the replacement disc is in the right place. After the procedure, the surgeon moves the tissue of the neck and throat back to its original location and seals the wound with stitches.
What happens during surgery?
There are seven steps to the procedure. The operation generally takes 1 to 3 hours.
Step 1: prepare the patient
You will lie on your back on the operative table and be given anesthesia. Once asleep, your neck area is cleansed and prepped. If a fusion is planned and your own bone will be used, the hip area is also prepped to obtain a bone graft. If a donor bone will be used, the hip incision is unnecessary.
Step 2: make an incision
A 2-inch skin incision is made on the right or left side of your neck (Fig. 2). The surgeon makes a tunnel to the spine by moving aside muscles in your neck and retracting the trachea, esophagus, and arteries. Finally, the muscles that support the front of the spine are lifted and held aside so the surgeon can clearly see the bony vertebrae and discs.
Step 3: locate the damaged disc
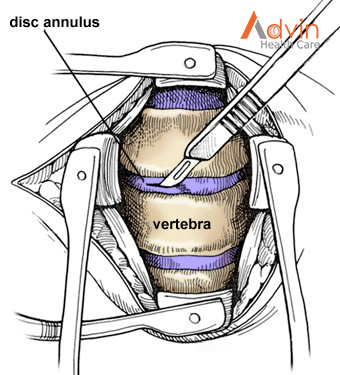
With the aid of a fluoroscope (a special X-ray), the surgeon passes a thin needle into the disc to locate the affected vertebra and disc. The vertebrae bones above and below the damaged disc are spread apart with a special retractor.
Step 4: remove the disc
The outer wall of the disc is cut (Fig. 3). The surgeon removes about 2/3 of your disc using small grasping tools, and then looks through a surgical microscope to remove the rest of the disc. The ligament that runs behind the vertebrae is removed to reach the spinal canal. Any disc material pressing on the spinal nerves is removed.
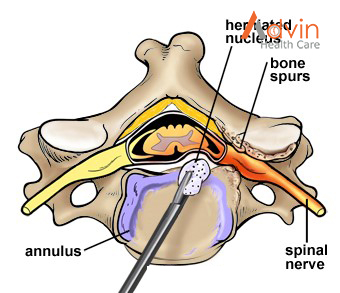
Step 5: decompress the nerve
Bone spurs that press on your nerve root are removed. The foramen, through which the spinal nerve exits, is enlarged with a drill (Fig. 4). This procedure, called a foraminotomy, gives your nerves more room to exit the spinal canal.
Step 6. prepare a bone graft fusion
Using a drill, the open disc space is prepared on the top and bottom by removing the outer cortical layer of bone to expose the blood-rich cancellous bone inside. This “bed” will hold the bone graft material that you and your surgeon selected:
- Bone graft from your hip.A skin and muscle incision is made over the crest of your hipbone. Next, a chisel is used to cut through the hard outer layer (cortical bone) to the inner layer (cancellous bone). The inner layer contains the bone-growing cells and proteins. The bone graft is then shaped and placed into the “bed” between the vertebrae (Fig. 5).
- Bone bank or fusion cage.A cadaver bone graft or bioplastic cage is filled with the leftover bone shavings containing bone-growing cells and proteins. The graft is then tapped into the shelf space.
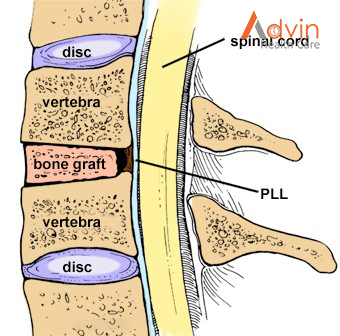
The bone graft is often reinforced with a metal plate screwed into the vertebrae to provide stability during fusion. An x-ray is taken to verify the position of the graft, plate, and screws (Fig. 6).
Alternative option: artificial disc replacement Instead of a bone graft or fusion cage, an artificial disc device is inserted into the empty disc space. In select patients, it may be beneficial to preserve motion. Talk to your doctor – not all insurance companies will pay for this new technology and out-of-pocket expenses may be incurred.
Step 7. close the incision The spreader retractors are removed.
The muscle and skin incisions are sutured together. Steri-Strips or biologic glue is placed across the incision.
Benefits of a Anterior Cervical Fusion Procedure
1. The “fusing” is a natural process.
Successful spinal decompression and fusion surgeries result in the end goal of joining two or more vertebrae together for the purpose of promoting stability and strength in the previously damaged area of the spine. However, there is a common misconception that the fusion itself takes place during the procedure. This is not the case. While all of the necessary preparatory work is completed during surgery (damaged disc and tissue are cleaned out, new bone implant is placed between the vertebrae, etc.) the fusing of the vertebrae is left to take place as a natural healing process post-surgery. This is part of what makes this procedure so successful as a long term solution. A proper recovery that results in a successful fusion will provide stability for the spine for years to come.
2. An anterior approach sometimes provides better access for your surgeon.
If there is a procedure specifically called “anterior cervical fusion” then you might assume that there is also one that takes place from a posterior approach – and you would be right! So, what’s the difference between these two surgeries? And why is the anterior incision sometimes prefered? The choice of how to approach the spine is made by assessing the location of the compressive pathology. Depending on where the problem issue is and how the cervical region of the spine is aligned, your surgeon will make a call concerning whether the surgery would be more successful if approached anteriorly or posteriorly.
3. This approach to cervical surgery offers a quick recovery.
Besides the advantage to the surgeon, there is also a benefit to the patient who undergoes an anterior spinal decompression and fusion surgery. If the spinal injury is addressed before the point of irreversible damage, patients tend to heal quickly and experience a significant degree of relief from pain. In fact, one of the most impressive aspects of anterior cervical fusion procedures is that most patients are able to leave the hospital the very next day (or, at least within 2-3 days).
4. Patients experience significant relief of pain and other symptoms.
Of course, the conversation about the benefits of decompression and fusion surgery would not be complete without discussing the most obvious reason any patient would consider having this procedure done in the first place – pain relief! Cervical herniated discs and osteoarthritis are some of the more common causes of severe neck and arm pain. These conditions are also often associated with other symptoms as well, such as numbness, tingling or weakness. A successful decompression and anterior cervical fusion procedure can correct the root issue and provide relief of the associated pain and other symptoms.


