In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.
During IVF, mature eggs are collected (retrieved) from ovaries and fertilized by sperm in a lab. Then the fertilized egg (embryo) or eggs (embryos) are transferred to a uterus. One full cycle of IVF takes about three weeks. Sometimes these steps are split into different parts and the process can take longer.
IVF is the most effective form of assisted reproductive technology. The procedure can be done using a couple’s own eggs and sperm. Or IVF may involve eggs, sperm or embryos from a known or anonymous donor. In some cases, a gestational carrier — someone who has an embryo implanted in the uterus — might be used.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. In addition, IVF can be time-consuming, expensive and invasive. If more than one embryo is transferred to the uterus, IVF can result in a pregnancy with more than one fetus (multiple pregnancy).
Your doctor can help you understand how IVF works, the potential risks and whether this method of treating infertility is right for you.
What Is IVF?
IVF is an assisted reproductive technology ideal for couples who haven’t been able to conceive naturally. The IVF process mimics natural fertilisation by uniting sperm and eggs in a petri dish, in a fastidiously controlled, carefully sanitised environment. Then, once fertilisation occurs, one or more embryos is transferred to the uterus for implantation.
Why it’s done

In vitro fertilization (IVF) is a treatment for infertility or genetic problems. If IVF is performed to treat infertility, you and your partner might be able to try less-invasive treatment options before attempting IVF, including fertility drugs to increase production of eggs or intrauterine insemination — a procedure in which sperm are placed directly in the uterus near the time of ovulation.
Sometimes, IVF is offered as a primary treatment for infertility in women over age 40. IVF can also be done if you have certain health conditions. For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.
- Endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are benign tumors in the uterus. They are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
- Previous tubal sterilization or removal. Tubal ligation is a type of sterilization in which the fallopian tubes are cut or blocked to permanently prevent pregnancy. If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery.
- Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg. If semen abnormalities are found, a visit to an infertility specialist might be needed to see if there are correctable problems or underlying health concerns.
- Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, you may be candidates for preimplantation genetic testing — a procedure that involves IVF. After the eggs are harvested and fertilized, they’re screened for certain genetic problems, although not all genetic problems can be found. Embryos that don’t contain identified problems can be transferred to the uterus.
- Fertility preservation for cancer or other health conditions. If you’re about to start cancer treatment — such as radiation or chemotherapy — that could harm your fertility, IVF for fertility preservation may be an option. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
Women who don’t have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy (gestational carrier). In this case, the woman’s eggs are fertilized with sperm, but the resulting embryos are placed in the gestational carrier’s uterus.
Who Is Best Suited for IVF?
IVF is often considered a last-line treatment when other treatments like ovulation induction and intrauterine insemination (IUI) have failed. For couples with some forms of infertility, it may be recommended as a first-line treatment. Some cases best suited for IVF include:
- Tubal infertility: A case of blocked or absent fallopian tubes, which prevents sperm from travelling to the egg, or blocks a fertilised egg from reaching the uterus
- Compromised sperm function: Problems with sperm production, morphology or motility
- Polycystic ovarian syndrome: A hormonal disorder that impedes ovulation and increases the risk of miscarriage
- Endometriosis: A condition where uterine tissue grows outside the uterus, causing scarring and adhesions
- Irregular menstrual cycles: Ovulatory dysfunction which leads to compromised egg quality and infrequent ovulation, minimising chances of conception
- Surrogacy: If a gestational carrier is opted for, IVF is essential to transfer the embryo to the surrogate’s uterus.
How you prepare
Before beginning a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screenings, including:
- Ovarian reserve testing. To determine the quantity and quality of your eggs, your doctor might test the concentration of follicle-stimulating hormone (FSH), estradiol (estrogen) and anti-mullerian hormone in your blood during the first few days of your menstrual cycle. Test results, often used together with an ultrasound of your ovaries, can help predict how your ovaries will respond to fertility medication.
- Semen analysis. If not done as part of your initial fertility evaluation, your doctor will conduct a semen analysis shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for infectious diseases, including HIV.
- Practice (mock) embryo transfer. Your doctor might conduct a mock embryo transfer to determine the depth of your uterine cavity and the technique most likely to successfully place the embryos into your uterus.
- Uterine exam. Your doctor will examine the inside lining of the uterus before you start IVF. This might involve a sonohysterography — in which fluid is injected through the cervix into your uterus — and an ultrasound to create images of your uterine cavity. Or it might include a hysteroscopy — in which a thin, flexible, lighted telescope (hysteroscope) is inserted through your vagina and cervix into your uterus.
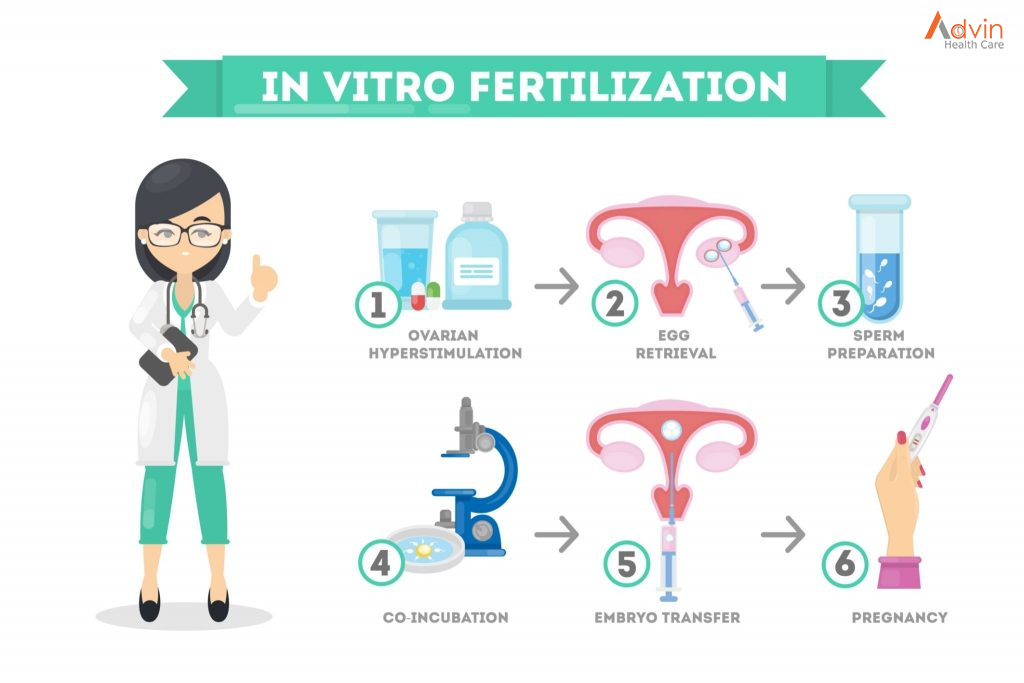
What Are the Steps of IVF?
IVF usually follows a seven-step process, given below.
Step 1. Ovulation Induction
As a first step, fertility medication is administered to encourage the maturation of ovarian follicles. During this time, the fertility specialist will closely monitor hormone levels and ovarian progress to ensure the follicles are responding optimally.
Step 2. Egg Collection
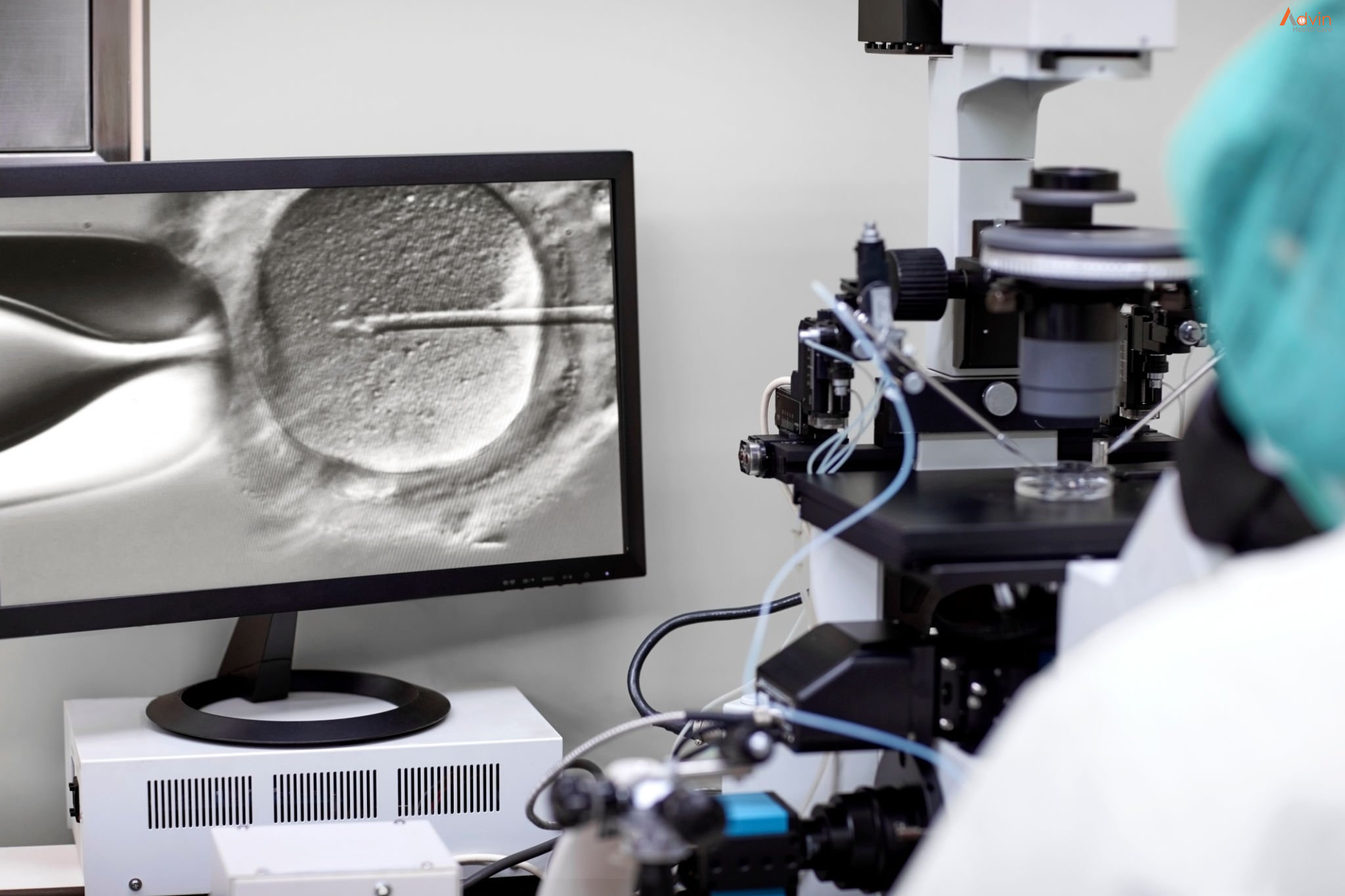
Egg collection is a straightforward procedure, performed under anaesthesia. A fine needle is passed through the vagina to retrieve eggs from mature follicles.
Step 3. Fertilisation
Once the eggs and sperm have been collected, they are fused together to create several embryos. This process may or may not be performed using additional technologies, including PGS, PGD and ICSI.
Step 4. Embryo Development
Embryos are left to develop over a period of four to five days, until they have reached the blastocyst stage. They are then graded for quality and integrity.
Step 5. Embryo Transfer
Once the embryo is four or five days old, and has become a blastocyst, it is transferred to the uterus for implantation. You can choose to cryopreserve your remaining embryos for future use.
Step 6. Pregnancy
Two weeks after your embryo transfer, comes judgement day – the day you finally discover whether your procedure has been successful. If it has, it’s time for a little celebration. And two weeks later, time for an ultrasound scan to check for a heartbeat.
Step 7. Follow-Ups
Regular follow-ups are recommended after a successful IVF cycle, to rule out potential complications. You can use this time to ask your doctor questions and prepare yourself for the wonderful months ahead!