Hemodialysis
In haemodialysis, a machine filters wastes, salts and fluid from your blood when your kidneys are no longer healthy enough to do this work adequately. Hemodialysis (he-moe-die-AL-uh-sis) is one way to treat advanced kidney failure and can help you carry on an active life despite failing kidneys.
With haemodialysis, you’ll need to:
- Follow a strict treatment schedule
- Take medications regularly
- Make changes in your diet
Haemodialysis is a serious responsibility, but you don’t have to shoulder it alone. You’ll work closely with your health care team, including a kidney specialist and other professionals with experience managing haemodialysis. You may be able to do haemodialysis at home.
Why it’s done
Your doctor will help determine when you should start hemodialysis based on several factors, including your:
- Overall health
- Kidney function
- Signs and symptoms
- Quality of life
- Personal preferences
You might notice signs and symptoms of kidney failure (uremia), such as nausea, vomiting, swelling or fatigue. Your doctor uses your estimated glomerular filtration rate (eGFR) to measure your level of kidney function. Your eGFR is calculated using your blood creatinine test results, sex, age and other factors. A normal value varies with age. This measure of your kidney function can help to plan your treatment, including when to start haemodialysis.
Haemodialysis can help your body control blood pressure and maintain the proper balance of fluid and various minerals — such as potassium and sodium — in your body. Normally, haemodialysis begins well before your kidneys have shut down to the point of causing life-threatening complications.
Common causes of kidney failure include:
- Diabetes
- High blood pressure (hypertension)
- Kidney inflammation (glomerulonephritis)
- Kidney cysts (polycystic kidney disease)
- Inherited kidney diseases
- Long-term use of nonsteroidal anti-inflammatory drugs or other medications that could harm the kidneys
However, your kidneys may shut down suddenly (acute kidney injury) after a severe illness, complicated surgery, heart attack or other serious problem. Certain medications also can cause kidney injury.
Some people with severe long-standing (chronic) kidney failure may decide against starting dialysis and opt for a different path. Instead, they may choose maximal medical therapy, also called maximum conservative management or palliative care. This therapy involves active management of complications of advanced chronic kidney disease, such as fluid overload, high blood pressure and anemia, with a focus on supportive management of symptoms that affect quality of life.
Other people may be candidates for a pre-emptive kidney transplant, instead of starting on dialysis. Ask your health care team for more information about your options. This is an individualized decision because benefits of dialysis may vary, depending on your particular health issues.
Haemodialysis Procedure
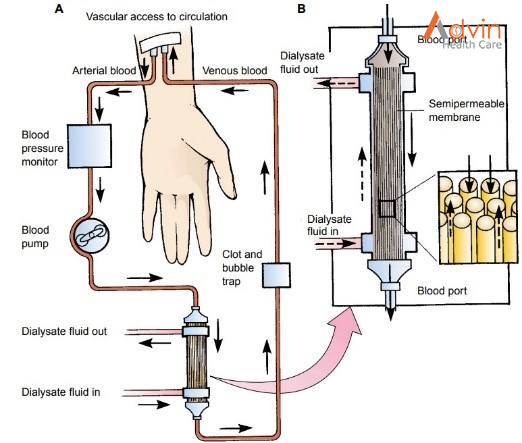
During treatments, you sit or recline in a chair while your blood flows through the dialyzer ― a filter that acts as an artificial kidney to clean your blood. You can use the time to watch TV or a movie, read, nap, or perhaps talk to your “neighbours” at the centre. If you receive haemodialysis at night, you can sleep during the procedure.
- Preparation: Your weight, blood pressure, pulse and temperature are checked. The skin covering your access site — the point where blood leaves and then renters your body during treatment — is cleansed.
- Starting: During haemodialysis, two needles are inserted into your arm through the access site and taped in place to remain secure. Each needle is attached to a flexible plastic tube that connects to a dialyzer. Through one tube, the dialyzer filters your blood a few ounces at a time, allowing wastes and extra fluids to pass from your blood into a cleansing fluid called dialysate. The filtered blood returns to your body through the second tube.
- Symptoms: You may experience nausea and abdominal cramps as excess fluid is pulled from your body — especially if you have gained a significant amount of fluid in between dialysis sessions. If you’re uncomfortable during the procedure, ask your care team about minimizing side effects by such measures as adjusting the speed of your haemodialysis, your medication or your haemodialysis fluids.
- Monitoring: Because blood pressure and heart rate can fluctuate as excess fluid is drawn from your body, your blood pressure and heart rate will be checked several times during each treatment.
- Finishing: When haemodialysis is completed, the needles are removed from your access site and a pressure dressing is applied to the site to prevent bleeding. Your weight may be recorded again. Then you’re free to go about your usual activities until your next session.
Benefits of haemodialysis
Aside from allowing people to continue living a relatively normal life, haemodialysis has other benefits, such as:
Haemodialysis requires less time than peritoneal dialysis
Haemodialysis treatments may occur at a hospital, dialysis center or your own home three times a week, with each session lasting between three and five hours. This leaves most of the week dialysis-free. By contrast, peritoneal dialysis takes between 10 and 12 hours every day.
Haemodialysis carries a relatively low risk of infection
Haemodialysis uses and arteriovenous (AV) fistula, which is the gold standard vascular access used to access a person’s blood. Common complications of peritoneal dialysis include infections of the abdominal lining or at the site where the catheter is inserted to carry the cleansing fluid.
Haemodialysis requires less surgical interventions
AV fistulas for dialysis last many years, longer than transplanted kidneys and catheters for peritoneal dialysis. This type of dialysis does not typically require additional surgeries.


