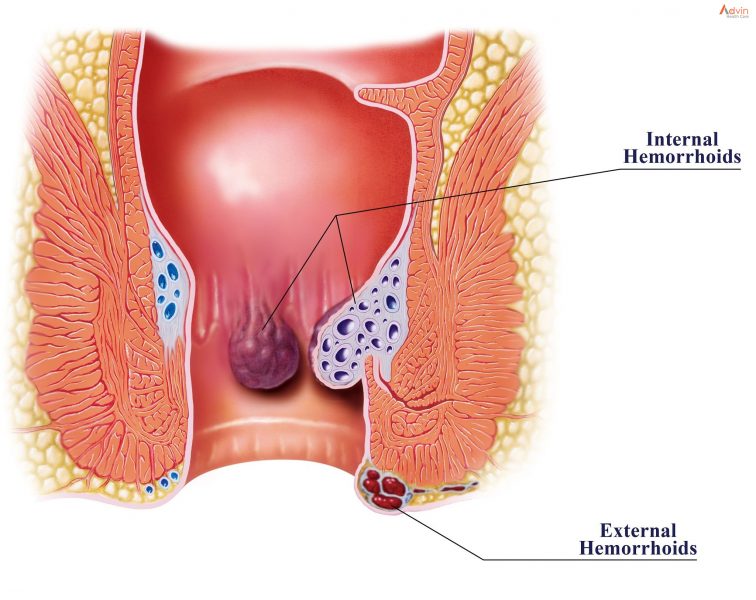
Hemorrhoids (HEM-uh-roids), also called piles, are swollen veins in your anus and lower rectum, similar to varicose veins. Hemorrhoids can develop inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids).
Nearly three out of four adults will have hemorrhoids from time to time. Hemorrhoids have a number of causes, but often the cause is unknown.
Fortunately, effective options are available to treat hemorrhoids. Many people get relief with home treatments and lifestyle changes.
What causes hemorrhoids?
Straining puts pressure on veins in your anus or rectum, causing hemorrhoids. You might think of them as varicose veins that affect your bottom.
Any sort of straining that increases pressure on your belly or lower extremities can cause anal and rectal veins to become swollen and inflamed. Hemorrhoids may develop due to:
- Pelvic pressure from weight gain, especially during pregnancy.
- Pushing hard to have a bowel movement (poop) because of constipation.
- Straining to lift heavy objects or weightlifting.
What are the symptoms of hemorrhoids?
Internal hemorrhoids rarely cause pain (and typically can’t be felt) unless they prolapse. Many people with internal hemorrhoids don’t know they have them because they don’t have symptoms.
If you have symptoms of internal hemorrhoids, you might see blood on toilet paper, in your stool or in the toilet bowl. These are signs of rectal bleeding.
Signs of external hemorrhoids include:
- Itchy anus.
- Hard lumps near your anus that feel sore or tender.
- Pain or ache in your anus, especially when you sit.
- Rectal bleeding.
Prolapsed hemorrhoids can be painful and uncomfortable. You may be able to feel them bulging outside of your anus and gently push them back inside.
How are hemorrhoids diagnosed?
A healthcare provider diagnoses hemorrhoids based on symptoms and a physical exam. You may also have:
- Digital rectal exam: Your provider inserts a gloved, lubricated finger into your rectum to feel for swollen veins.
- Anoscopy: Your provider uses an anoscope (lighted tube) to view the lining of your anus and rectum.
- Sigmoidoscopy: Your provider uses a sigmoidoscope (lighted tube with a camera) to view inside the lower (sigmoid) part of your colon and rectum. Procedure types include flexible sigmoidoscopy and rigid sigmoidoscopy (proctoscopy).
These tests may be uncomfortable but aren’t painful. They typically take place in a doctor’s office or outpatient center without anesthesia. You go home the same day.
Your provider may perform a colonoscopy to confirm findings from other tests or check for signs of colon cancer. This outpatient procedure requires anesthesia.
What are the complications of hemorrhoids?
Hemorrhoids can be uncomfortable and painful, but they don’t tend to cause serious problems. Rarely, people with hemorrhoids develop:
- Anemia.
- Blood clots in external hemorrhoids.
- Infection.
- Skin tags (flap of tissue that hangs off skin).
- Strangulated hemorrhoids (muscles in the anus cut off blood flow to a prolapsed internal hemorrhoid).
How can I treat hemorrhoids at home?
Hemorrhoids often go away on their own without treatment. Symptoms like pain and bleeding may last one week or slightly longer. In the meantime, you can take these steps to ease symptoms:
- Apply over-the-counter medications containing lidocaine, witch hazel or hydrocortisone to the affected area.
- Drink more water.
- Increase fiber intake through diet and supplements. Try to obtain at least 20 to 35 grams of daily fiber intake.
- Soak in a warm bath for 10 to 20 minutes a day.
- Soften stool by taking laxatives.
- Take nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation.
- Use toilet paper with lotion or flushable wet wipes to gently pat and clean your bottom after pooping. You can also use a tissue or washcloth moistened with water. (Discard wipes in the trash, not by flushing. Launder washcloths separately in hot water to avoid spreading infections often found in poop.)
How do healthcare providers treat hemorrhoids?
You should see your healthcare provider if symptoms get worse or interfere with your daily life or sleep. Also, seek help if signs don’t improve after a week of at-home treatments. Your provider may treat hemorrhoids with:
- Rubber band ligation: A small rubber band placed around the base of a hemorrhoid cuts off blood supply to the vein.
- Electrocoagulation: An electric current stops blood flow to a hemorrhoid.
- Infrared coagulation: A small probe inserted into the rectum transmits heat to get rid of the hemorrhoid.
- Sclerotherapy: A chemical injected into the swollen vein destroys hemorrhoid tissue.
Surgical treatments include:
- Hemorrhoidectomy: Surgery removes large external hemorrhoids or prolapsed internal ones.
- Hemorrhoid stapling: A stapling instrument removes an internal hemorrhoid. Or it pulls a prolapsed internal hemorrhoid back inside of your anus and holds it there.