Knee Replacement
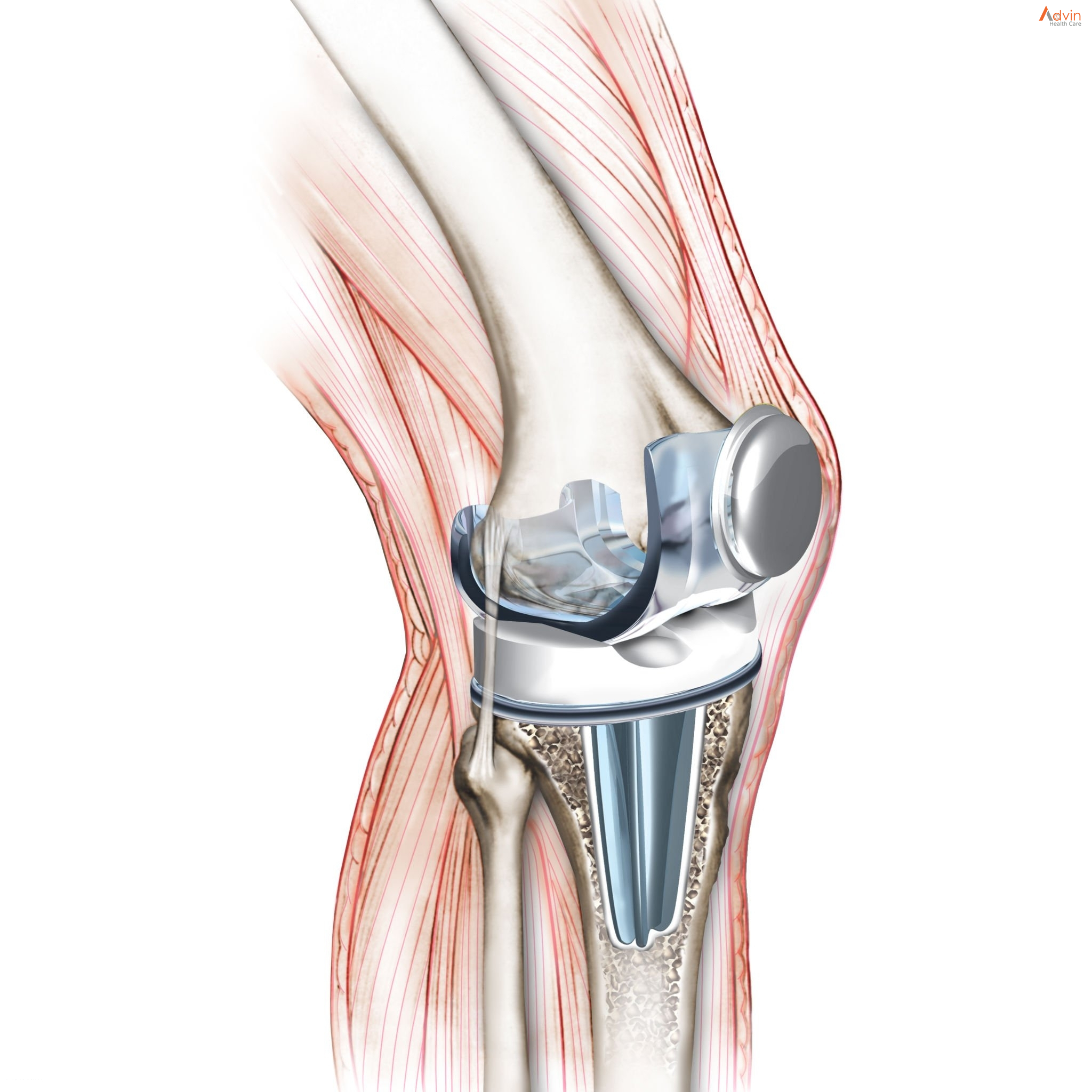
Knee replacement surgery — also known as knee arthroplasty (ARTH-row-plas-tee) — can help relieve pain and restore function in severely diseased knee joints. The procedure involves cutting away damaged bone and cartilage from your thighbone, shinbone and kneecap and replacing it with an artificial joint (prosthesis) made of metal alloys, high-grade plastics and polymers.
In determining whether a knee replacement is right for you, an orthopedic surgeon assesses your knee’s range of motion, stability and strength. X-rays help determine the extent of damage.
Your doctor can choose from a variety of knee replacement prostheses and surgical techniques, considering your age, weight, activity level, knee size and shape, and overall health.
Anatomy of the knee
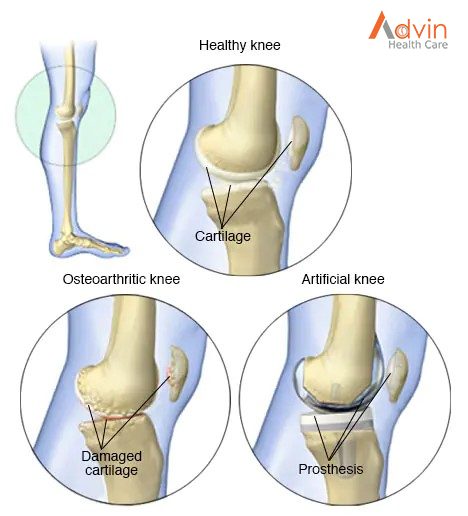
Joints are the areas where 2 or more bones meet. Most joints are mobile, allowing the bones to move. Basically, the knee is 2 long leg bones held together by muscles, ligaments, and tendons. Each bone end is covered with a layer of cartilage that absorbs shock and protects the knee.
There are 2 groups of muscles involved in the knee, including the quadriceps muscles (located on the front of the thighs), which straighten the legs, and the hamstring muscles (located on the back of the thighs), which bend the leg at the knee.
Tendons are tough cords of connective tissue that connect muscles to bones. Ligaments are elastic bands of tissue that connect bone to bone. Some ligaments of the knee provide stability and protection of the joints, while other ligaments limit forward and backward movement of the tibia (shin bone).
The knee consists of the following:
- Tibia: This is the shin bone or larger bone of the lower leg.
- Femur: This is the thighbone or upper leg bone.
- Patella: This is the kneecap.
- Cartilage: A type of tissue that covers the surface of a bone at a joint. Cartilage helps reduce the friction of movement within a joint.
- Synovial membrane: A tissue that lines the joint and seals it into a joint capsule. The synovial membrane secretes synovial fluid (a clear, sticky fluid) around the joint to lubricate it.
- Ligament: A type of tough, elastic connective tissue that surrounds the joint to give support and limits the joint’s movement.
- Tendon: A type of tough connective tissue that connects muscles to bones and helps to control movement of the joint.
- Meniscus: A curved part of cartilage in the knees and other joints that acts as a shock absorber, increases contact area, and deepens the knee joint.
What is knee replacement and why is it useful?
Knee replacement is a kind of arthroplasty. Arthroplasty literally means “the surgical repair of a joint,” and it involves the surgical reconstruction and replacement of degenerated joints, using artificial body parts, or prosthetics.
When the articular cartilage of the knee becomes damaged or worn, it becomes painful and the knee is hard to move. Instead of sliding over each other, the bones rub and crush together.
With a prosthesis, the patient will feel less pain, and the knee will move properly.
Why have knee replacement surgery?
There are three common reasons for the procedure:
Osteoarthritis: this type of arthritis is age related, caused by the normal wear and tear of the knee joint. It mostly affects patients aged over 50 years, but younger people may have it.
Osteoarthritis is caused by inflammation, breakdown, and the gradual and eventual loss of cartilage in the joints. Over time, the cartilage wears down and the bones rub together. To compensate, the bones often grow thicker, but this results in more friction and more pain.
Rheumatoid arthritis: also called inflammatory arthritis, the membrane around the knee joint to become thick and inflamed. Chronic inflammation damages the cartilage, causing soreness and stiffness.
Post-traumatic arthritis: this type of arthritis is due to a severe knee injury. When the bones around the knee break or the ligaments tear, this will affect the knee cartilage.
Types of knee replacement surgery
Knee replacement can be total or partial.
Total knee replacement (TKR): Surgery involves the replacement of both sides of the knee joint. It is the most common procedure.
Surgery lasts between 1 and 3 hours. The individual will have less pain and better mobility, but there will be scar tissue, which can make it difficult to move and bend the knees.
Partial knee replacement (PKR): Partial replacement replaces only one side of the knee joint. Less bone is removed, so the incision is smaller, but it does not last as long as a total replacement.
PKR is suitable for people with damage to only one part of the knee. Post-operative rehabilitation is more straightforward, there is less blood loss and a lower risk of infection and blood clots.
The hospital stay and recovery period are normally shorter, and there is a higher chance of more natural movement.
What you can expect
Before the procedure
Knee replacement surgery requires anesthesia. Your input and preference help the team decide whether to use general anesthesia, which makes you unconscious, or spinal anesthesia, which leaves you awake but unable to feel pain from your waist down.
You’ll be given an intravenous antibiotic before, during and after the procedure to help prevent post-surgical infection. You might also be given a nerve block around your knee to numb it. The numbness wears off gradually after the procedure.
During the procedure
Your knee will be in a bent position to expose all surfaces of the joint. After making an incision about 6 to 10 inches (15 to 25 centimeters) long, your surgeon moves aside your kneecap and cuts away the damaged joint surfaces.
After preparing the joint surfaces, the surgeon attaches the pieces of the artificial joint. Before closing the incision, he or she bends and rotates your knee, testing it to ensure proper function. The surgery lasts about two hours.
After the procedure
You’ll be taken to a recovery room for one to two hours. How long you stay after surgery depends on your individual needs. Many people can go home that same day. Medications prescribed by your doctor should help control pain.
You’ll be encouraged to move your foot and ankle, which increases blood flow to your leg muscles and helps prevent swelling and blood clots. You’ll likely receive blood thinners and wear support hose or compression boots to further protect against swelling and clotting.
You’ll be asked to do frequent breathing exercises and gradually increase your activity level. A physical therapist will show you how to exercise your new knee. After you leave the hospital, you’ll continue physical therapy at home or at a center.
Do your exercises regularly, as instructed. For the best recovery, follow all of your care team’s instructions concerning wound care, diet and exercise.
Advin Knee Replacement Products
- Martin Cartilage Clamp
- Weitlaner Retractor
- Steel Ruler
- Freer Elevator Double Ended With Blunt Sharp Blades
- Blount Knee Retractor
- Smillie Meniscus Hook Retractor Blade
- Smillie Cartilage Knife
- Lowe-Breck Cartilage Knife, Straight Edge With Guards
- Downing Cartilage Knife Concave Edge With Guards
- Volkman Retractor
- Knife Handle
- Allis Tissue Forceps
- Sayre Periosteal Elevator
- Key Elevator
- Adson Dura Hook Blunt Blade
- Graham Nerve Hook Blunt
- Kelly Hemostatic Forceps Curved
- Mayo Scissors Tungsten Carbide Curved
- Metzenbaum Scissors Standard Curved
- Lister Bandage Scissors
- Thumb Tissue Forceps
- Adson Dressing Forceps
- Adson Tissue Forceps
- Tissue Forceps
- Mayo Scissors Tungsten Carbide Straight
- Rochester Ochsner Forceps Straight
- Backhaus Towel Clamp
- Webster Needle Holder
- Crile Wood Needle Holder
- Tungsten Carbide Jaws Serrated
- Senn Miller Retractor
- Volkman Retractor