Chronic Kidney Disease
Chronic kidney disease (CKD) means your kidneys are damaged and can’t filter blood the way they should. The disease is called “chronic” because the damage to your kidneys happens slowly over a long period of time. This damage can cause wastes to build up in your body. CKD can also cause other health problems.
The kidneys’ main job is to filter extra water and wastes out of your blood to make urine. To keep your body working properly, the kidneys balance the salts and minerals—such as calcium, phosphorus, sodium, and potassium—that circulate in the blood. Your kidneys also make hormones that help control blood pressure, make red blood cells, and keep your bones strong.
Kidney disease often can get worse over time and may lead to kidney failure. If your kidneys fail, you will need dialysis or a kidney transplant to maintain your health.
The sooner you know you have kidney disease, the sooner you can make changes to protect your kidneys.
What are the symptoms of CKD?
Early CKD may not have any symptoms
You may wonder how you can have CKD and feel fine. Our kidneys have a greater capacity to do their job than is needed to keep us healthy. For example, you can donate one kidney and remain healthy. You can also have kidney damage without any symptoms because, despite the damage, your kidneys are still doing enough work to keep you feeling well. For many people, the only way to know if you have kidney disease is to get your kidneys checked with blood and urine tests.
As kidney disease gets worse, a person may have swelling, called edema. Edema happens when the kidneys can’t get rid of extra fluid and salt. Edema can occur in the legs, feet, or ankles, and less often in the hands or face.
Symptoms of advanced CKD
- chest pain
- dry skin
- itching or numbness
- feeling tired
- headaches
- increased or decreased urination
- loss of appetite
- muscle cramps
- nausea
- shortness of breath
- sleep problems
- trouble concentrating
- vomiting
- weight loss
What is Haemodialysis?
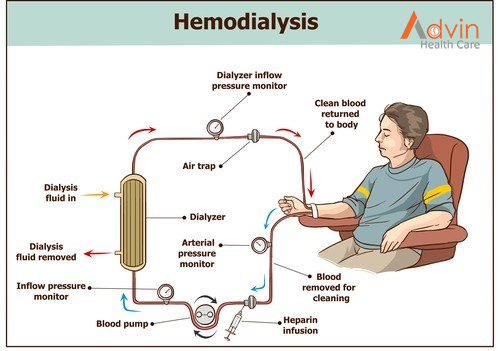
With haemodialysis, a machine removes blood from your body, filters it through a dialyzer (artificial kidney) and returns the cleaned blood to your body. This 3- to 5-hour process may take place in a hospital or a dialysis centre three times a week.
You can also do haemodialysis at home. You may need at-home treatments four to seven times per week for fewer hours each session. You may choose to do home haemodialysis at night while you sleep.
What happens before hemodialysis?
Before you start haemodialysis, you’ll undergo a minor surgical procedure to make it easier to access the bloodstream. You may have:
- Arteriovenous fistula (AV fistula): A surgeon connects an artery and vein in your arm.
- Arteriovenous graft (AV graft): If the artery and vein are too short to connect, your surgeon will use a graft (soft, hollow tube) to connect the artery and vein.
AV fistulas and grafts enlarge the connected artery and vein, which makes dialysis access easier. They also help blood flow in and out of your body faster.
If dialysis needs to happen quickly, your provider may place a catheter (thin tube) into a vein in your neck, chest or leg for temporary access.
Your provider will teach you how to prevent infections in your fistula or graft. This provider will also show you how to do haemodialysis at home if you choose to do so.
What happens during haemodialysis?
During haemodialysis, the dialysis machine:
- Removes blood from a needle in your arm.
- Circulates the blood through the dialyzer filter, which moves waste into a dialysis solution. This cleansing liquid contains water, salt and other additives.
- Returns filtered blood to your body through a different needle in your arm.
- Monitors your blood pressure to adjust how fast blood flows in and out of your body.
What is peritoneal dialysis?
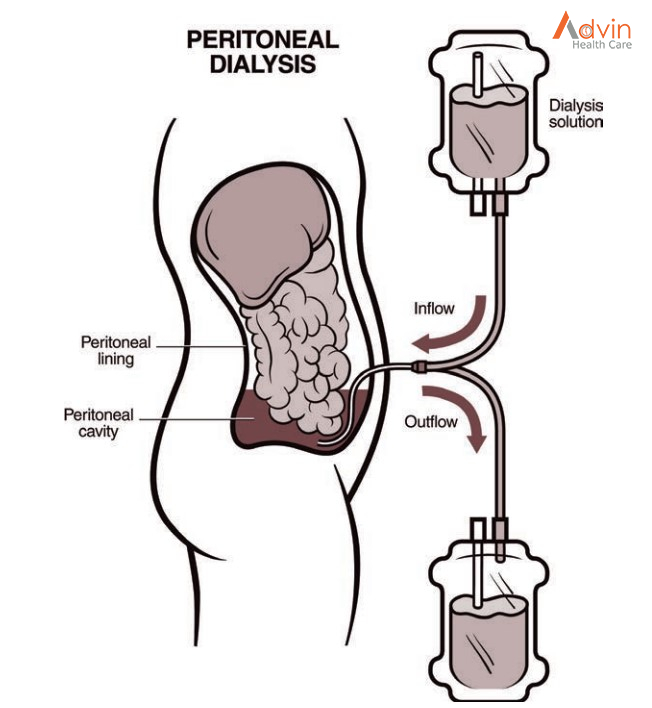
With peritoneal dialysis, tiny blood vessels inside the abdominal lining (peritoneum) filter blood through the aid of a dialysis solution. This solution is a type of cleansing liquid that contains water, salt and other additives.
Peritoneal dialysis takes place at home. There are two ways to do this treatment:
- Automated peritoneal dialysis uses a machine called a cycler.
- Continuous ambulatory peritoneal dialysis (CAPD) takes place manually.
What happens before peritoneal dialysis?
About three weeks before you start peritoneal dialysis, you’ll have a minor surgical procedure. A surgeon inserts a soft, thin tube (catheter) through your belly and into the peritoneum. This catheter stays in place permanently.
A healthcare provider will teach you how to perform peritoneal dialysis at home and prevent infections at the catheter site.
What happens during peritoneal dialysis?
During peritoneal dialysis, you:
- Connect the catheter to one branch of a Y-shaped tube. This tube connects to a bag that has dialysis solution. The solution flows through the tube and catheter into the peritoneal cavity.
- Disconnect the tube and catheter after about 10 minutes, when the bag is empty.
- Cap off the catheter.
- Go about your usual activities while the dialysis solution inside the peritoneal cavity absorbs waste and extra fluids from the body. This process can take 60 to 90 minutes.
- Remove the cap from the catheter and use the other branch of the Y-shaped tube to drain the fluid into a clean, empty bag.
- Repeat these steps up to four times a day. You sleep with the solution in your stomach all night.
- Some people prefer to do peritoneal dialysis at night. With automated peritoneal dialysis, a machine called a cycler pumps the fluid in and out of the body while you sleep.

ADVIN NEPHROLOGY / Haemodialysis SETUP
We, Advin Provides international Quality Standards Products for Haemodialysis Product
- Haemodialysis Machine
- Dialysis Chair
- RO Plant
- Bicarbonate Mixture
- Dialyzer
- Blood Line set
- AVF Needle
- Haemodialysis Double / Triple lumen Catheter Kit
- Acid Concentrate Part A Liquid / Solid
- Bicarbonate Part B Liquid / solid
- Bicarbonate Bi-Bag
- Bicarbonate Bi-Cart
- Hot Disaffection
- Cold Sterilant
- Peritoneal Dialysis Kit
- Heparin
- EPO Injection