Polycystic ovary syndrome (PCOS) is a problem with hormones that happens during the reproductive years. If you have PCOS, you may not have periods very often. Or you may have periods that last many days. You may also have too much of a hormone called androgen in your body.
With PCOS, many small sacs of fluid develop along the outer edge of the ovary. These are called cysts. The small fluid-filled cysts contain immature eggs. These are called follicles. The follicles fail to regularly release eggs.
The exact cause of PCOS is unknown. Early diagnosis and treatment along with weight loss may lower the risk of long-term complications such as type 2 diabetes and heart disease.
What is polycystic ovarian syndrome?
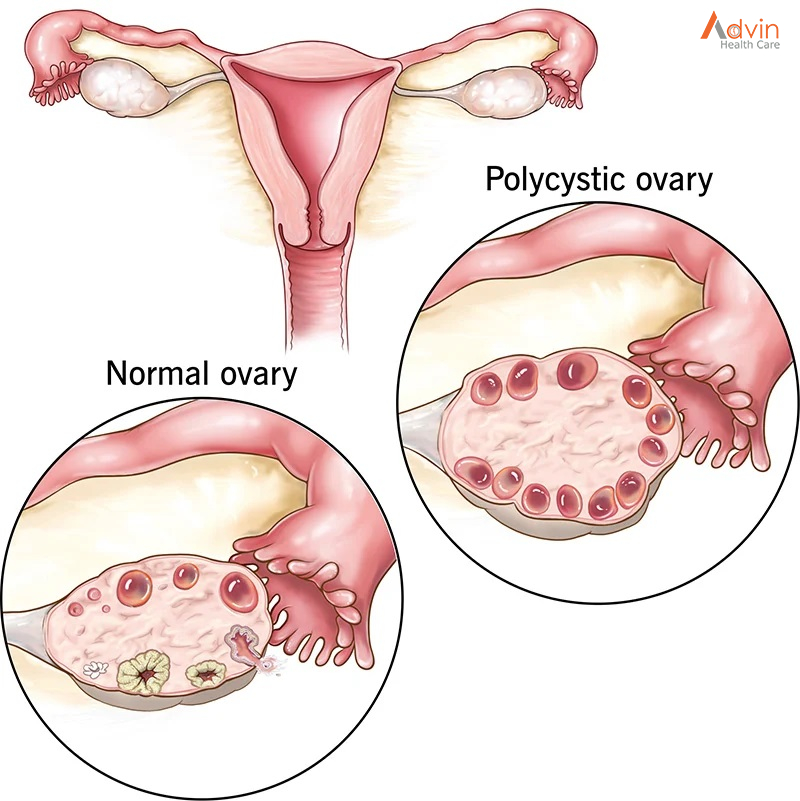
Polycystic ovarian syndrome (PCOS) is a hormonal imbalance caused by the ovaries (the organ that produces and releases eggs) creating excess male hormones. If you have PCOS, your ovaries produce unusually high levels of hormones called androgens. This causes your reproductive hormones to become imbalanced. As a result, people with PCOS often have erratic menstrual cycles, missed periods and unpredictable ovulation. Small cysts may develop on your ovaries (fluid-filled sacs) due to lack of ovulation (anovulation). However, despite the name “polycystic,” you do not need to have cysts on your ovaries to have PCOS.
PCOS is one of the most common causes of female infertility. It can also increase your risk for other health conditions. Your healthcare provider can treat PCOS based on your symptoms and if you have plans for having children.
Who can get PCOS?
A woman can get PCOS any time after puberty. Most people are diagnosed in their 20s or 30s when they are trying to get pregnant. You may have a higher chance of getting PCOS if you are overweight or have obesity, or if other people in your family have PCOS.
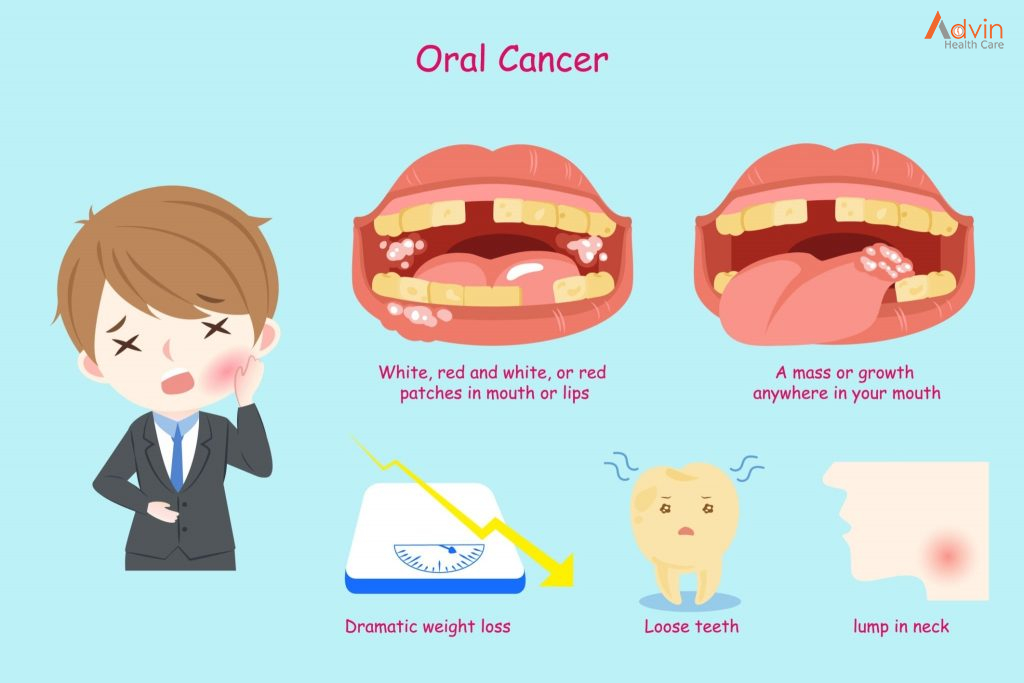
What are the symptoms of PCOS?
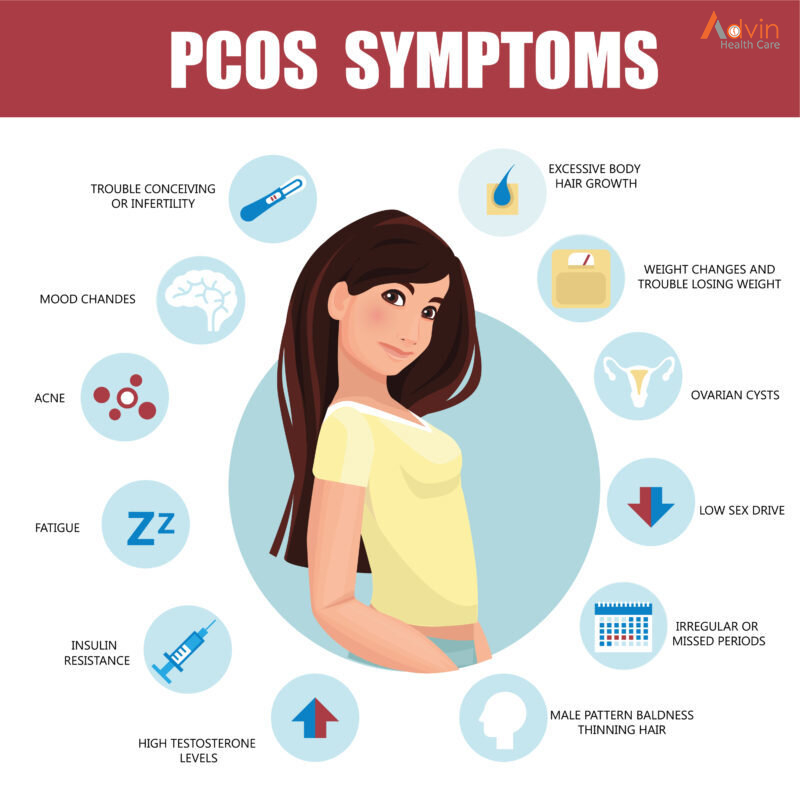
The symptoms of PCOS may include:
- Missed periods, irregular periods, or very light periods
- Ovaries that are large or have many cysts
- Excess body hair, including the chest, stomach, and back (hirsutism)
- Weight gain, especially around the belly (abdomen)
- Acne or oily skin
- Male-pattern baldness or thinning hair
- Infertility
- Small pieces of excess skin on the neck or armpits (skin tags)
- Dark or thick skin patches on the back of the neck, in the armpits, and under the breasts
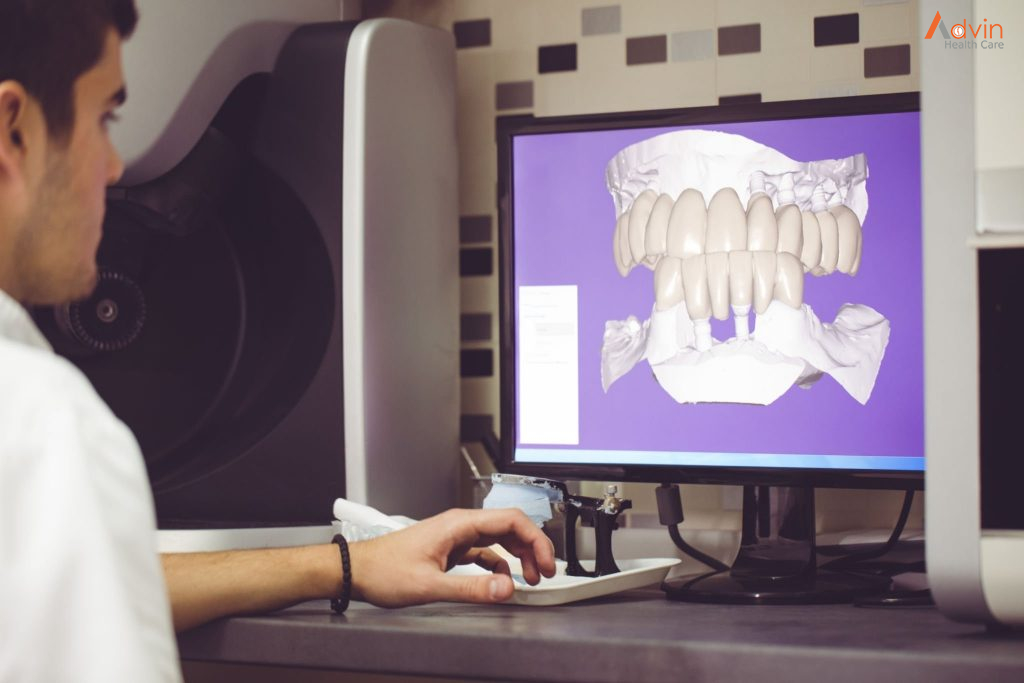
How is PCOS diagnosed?
Your health care provider will ask about your medical history and your symptoms. You will also have a physical exam. This will likely include a pelvic exam. This exam checks the health of your reproductive organs, both inside and outside your body.
Some of the symptoms of PCOS are like those caused by other health problems. Because of this, you may also have tests such as:
- This test uses sound waves and a computer to create images of blood vessels, tissues, and organs. This test is used to look at the size of the ovaries and see if they have cysts. The test can also look at the thickness of the lining of the uterus (endometrium).
- Blood tests. These look for high levels of androgens and other hormones. Your health care provider may also check your blood glucose levels. And you may have your cholesterol and triglyceride levels checked.
Hat is the main cause of polycystic ovarian syndrome?
The exact cause of PCOS is unknown. There is evidence that genetics play a role. Several other factors also play a role in causing PCOS:
- Higher levels of male hormones called androgens: High androgen levels prevent the ovaries from releasing eggs (ovulation), which causes irregular menstrual cycles. Irregular ovulation can also cause small, fluid-filled sacs to develop in the ovaries. High androgen also causes acne and excess hair growth in women.
- Insulin resistance: Increased insulin levels cause the ovaries to make and release male hormone (androgens). Increased male hormone, in turn, suppress ovulation and contribute to other symptoms of PCOS. Insulin helps your body processes glucose (sugar) and uses it for energy. Insulin resistance means your body doesn’t process insulin correctly, leading to high glucose levels in your blood. Not all individuals with insulin resistance have an elevated glucose or diabetes, but insulin resistance can lead to diabetes. Having overweight orobesity can also contribute to insulin resistance. An elevated insulin level, even if your blood glucose is normal, can indicate insulin resistance.
- Low–grade inflammation: People with PCOS tend to have chronic low-grade inflammation. Your healthcare provider can perform blood tests that measure levels of C-reactive protein (CRP) and white blood cells, which can indicate the level of inflammation in your body.
How is PCOS treated?
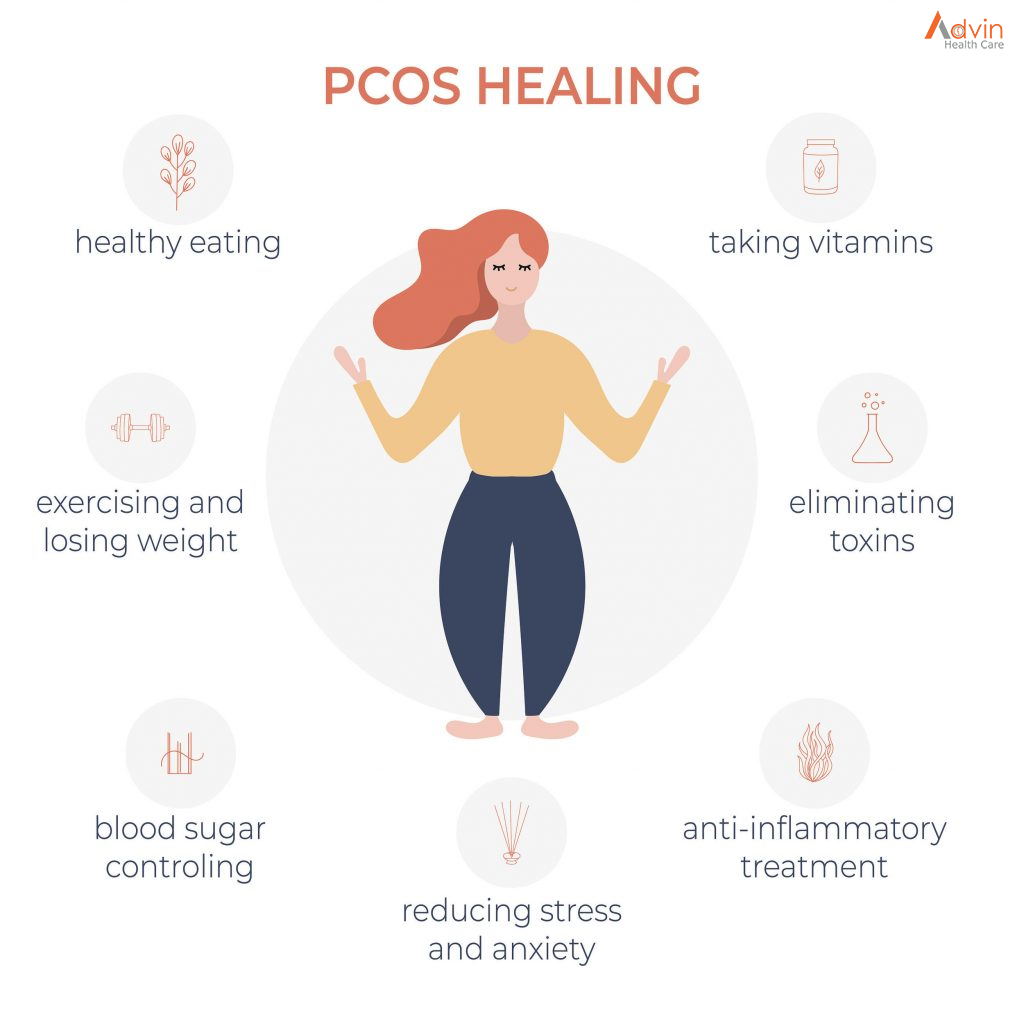
Treatment for PCOS depends on a number of factors. These may include your age, how severe your symptoms are, and your overall health. The type of treatment may also depend on whether you want to become pregnant in the future.
If you do plan to become pregnant, your treatment may include:
- A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
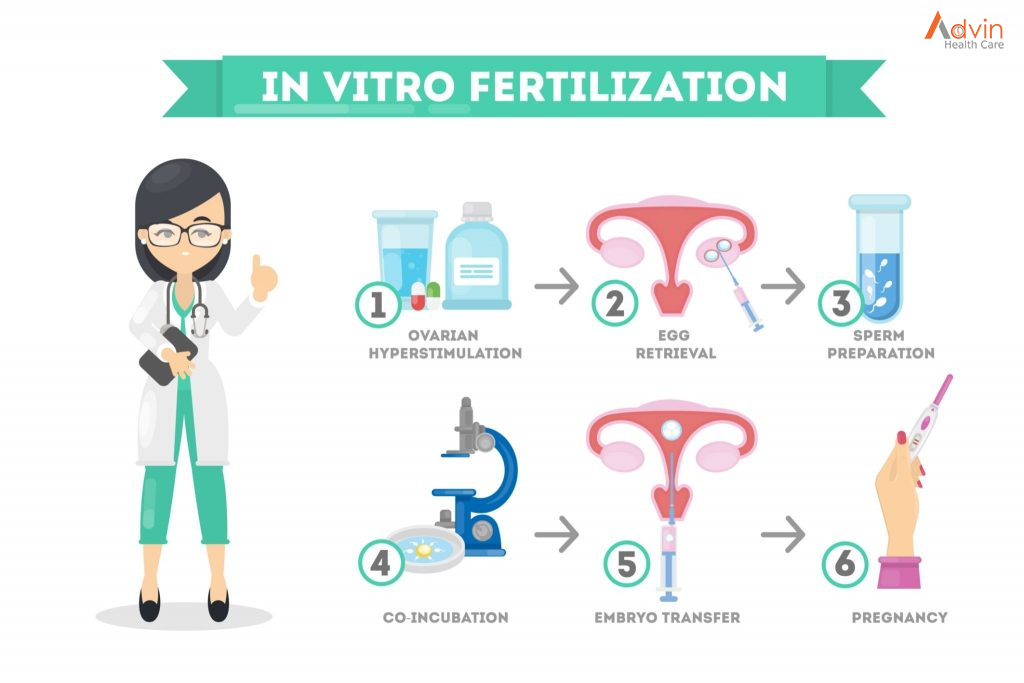
- Medications to cause ovulation.Medications can help the ovaries to release eggs normally. These medications also have certain risks. They can increase the chance for a multiple birth (twins or more). And they can cause ovarian hyperstimulation. This is when the ovaries release too many hormones. It can cause symptoms such as abdominal bloating and pelvic pain.
If you do not plan to become pregnant, your treatment may include:
- Birth control pills. These help to control menstrual cycles, lower androgen levels, and reduce acne.
- Diabetes medication. This is often used to lower insulin resistance in PCOS. It may also help reduce androgen levels, slow hair growth, and help you ovulate more regularly.
- A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
- Medications to treat other symptoms. Some medications can help reduce hair growth or acne.
When should I seek medical care?
If you have missed or irregular periods, excess hair growth, acne, and weight gain, call your doctor for an evaluation.
Key points
- PCOS is a very common hormone problem for women of childbearing age.
- Women with PCOS may not ovulate, have high levels of androgens, and have many small cysts on the ovaries.
- PCOS can cause missed or irregular menstrual periods, excess hair growth, acne, infertility, and weight gain.
- Women with PCOS may be at higher risk for type 2 diabetes, high blood pressure, heart problems, and endometrial cancer.
- The types of treatment for PCOS may depend on whether or not a woman plans to become pregnant. Women who plan to become pregnant in the future may take different kinds of medications.
Next steps
Tips to help you get the most from a visit to your health care provider:
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.