Join Us at WHX Dubai 2026: Shaping the Future of Global Healthcare
Advin Health Care is proud to announce its participation in WHX Dubai 2026 (World Health Expo Dubai), one of the world’s most influential healthcare exhibitions. Scheduled to take place from 09–12 February, 2026 at the Dubai Exhibition Center, UAE, WHX Dubai brings together global healthcare leaders, manufacturers, innovators, and decision-makers under one roof.
As a trusted medical manufacturing and export brand, Advin Health Care looks forward to showcasing its comprehensive product portfolio and reaffirming its commitment to advancing patient care through quality, innovation, and reliability.
What Makes WHX Dubai 2026 a Global Healthcare Landmark
WHX Dubai is more than an exhibition—it is a global platform for collaboration, innovation, and growth in the healthcare industry. The event attracts thousands of healthcare professionals, hospital administrators, distributors, and policymakers from across the world.
At WHX Dubai 2026, visitors can expect:
-
Exposure to cutting-edge medical technologies and solutions
-
Opportunities to connect with global manufacturers and healthcare leaders
-
Insightful discussions on emerging trends, challenges, and advancements
-
A strong environment for building long-term business partnerships
With its global reach and strong focus on innovation, WHX Dubai provides the ideal stage for Advin Health Care to present its advanced medical solutions.
Advin Health Care at WHX Dubai 2026
At Advin Health Care, we are driven by a mission to deliver dependable, clinically efficient, and internationally compliant medical products. Our participation in WHX Dubai 2026 reflects our continued efforts to support hospitals, clinics, and healthcare providers worldwide with high-quality medical devices and consumables.
Our team will be present to:
-
Showcase our latest product developments
-
Discuss customized solutions for diverse clinical needs
-
Explore distribution and partnership opportunities
-
Share insights into our manufacturing capabilities and quality standards
-
Stand No.: N25.D39
Our Medical Product Portfolio
Advin Health Care supplies a wide and specialized range of medical products across multiple disciplines:
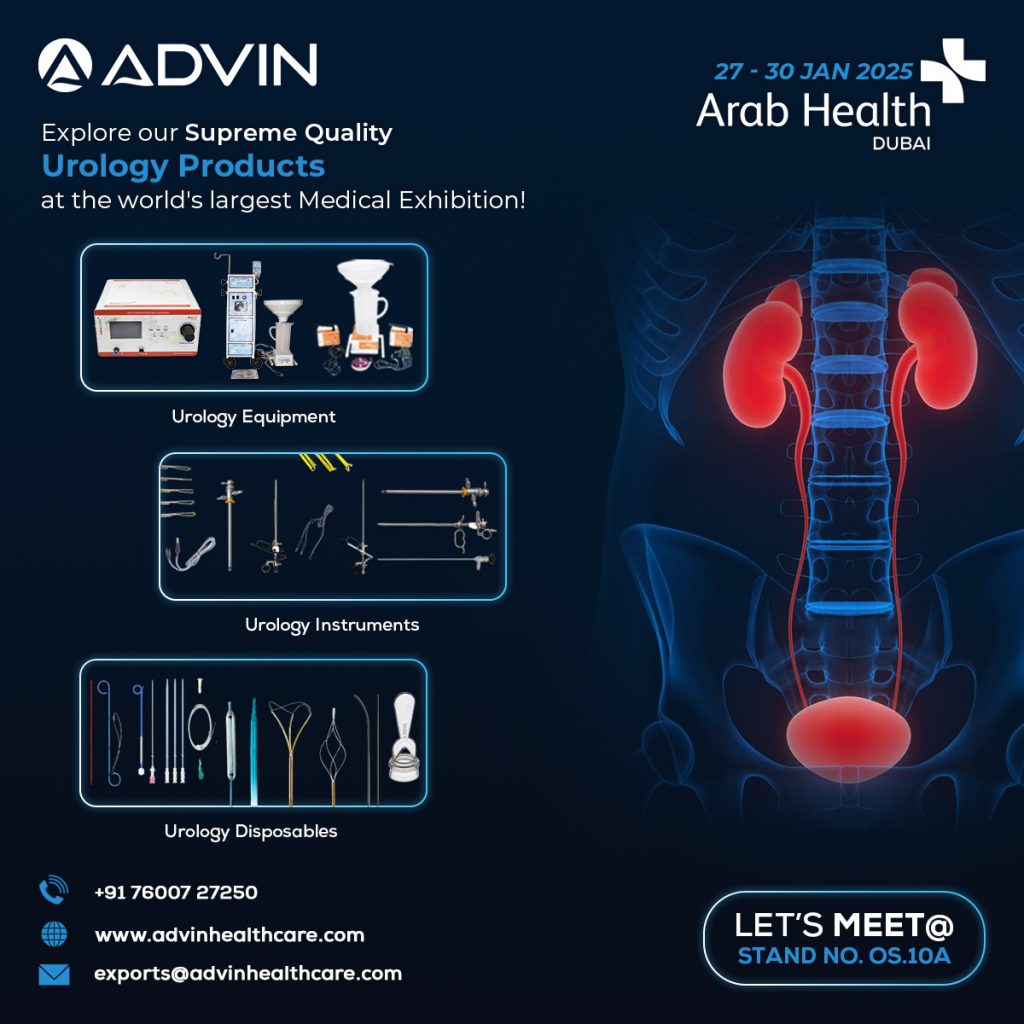
Urology
Focused on urinary and reproductive health, supporting accurate diagnosis and effective treatment.

Product Range:
Electrosurgical Equipment, TURP Resectoscope Products, Urology Instruments, Urology Equipment, Urology Disposables
Laparoscopy
Minimally invasive surgical solutions designed for precision, safety, and faster patient recovery.

Product Range:
Laparoscopy Equipment, Laparoscopic Hand Instruments, Laparoscopy Accessories
Gynecology
Comprehensive solutions supporting women’s reproductive health and surgical care.

Product Range:
Gynecology OT Tables, Uterine Manipulators, Gynecology Equipment, Gynecology Disposables
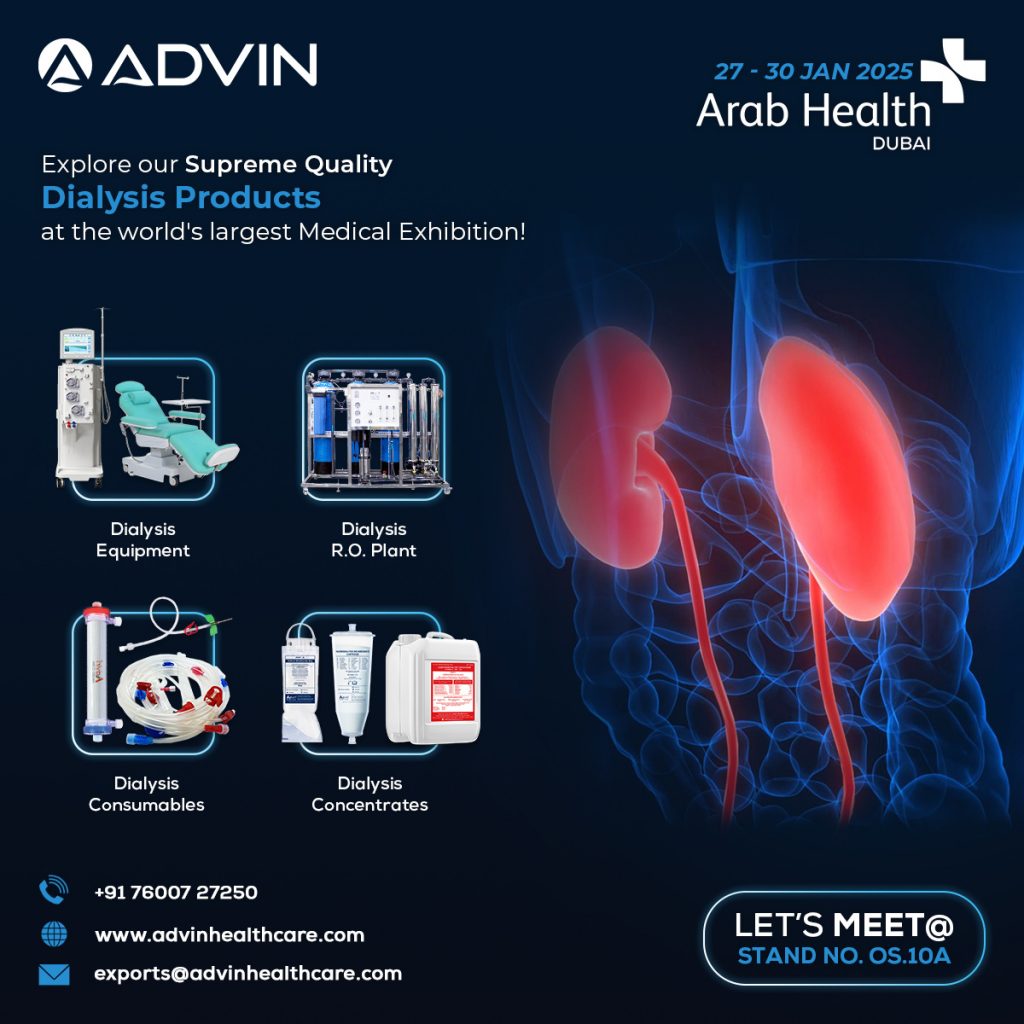
Nephrology
Advanced renal care solutions focused on safe and efficient dialysis therapy.

Product Range:
Dialysis Machines, Dialysis Equipment, Dialysis Concentrates, Dialysis Consumables, Dialysis Disinfectants
Cardiology
Reliable instruments and disposables supporting cardiovascular diagnosis and intervention.

Product Range:
Cardiology Instruments, Cardiology Disposables
Gastrology
Solutions for gastrointestinal diagnosis and therapeutic procedures.

Product Range:
Gastrology Equipment, Gastrology Disposables, ERCP Products
Why Visit Advin Health Care at WHX Dubai 2026
Whether you are a distributor, healthcare professional, or institutional buyer, visiting Advin Health Care at WHX Dubai 2026 offers the opportunity to:
-
Discover internationally trusted medical products
-
Explore cost-effective and scalable healthcare solutions
-
Engage directly with our expert team
-
Build long-term partnerships with a reliable manufacturing brand
We Look Forward to Meeting You
We warmly invite you to visit Advin Health Care at Stand No. N25.D39 during WHX Dubai 2026. Let’s connect, collaborate, and work together toward advancing global healthcare with quality-driven medical solutions.
WHX Dubai 2026 (World Health Expo Dubai)
Dates: 09–12 February 2026
Venue: Dubai Exhibition Center, UAE
Stand No.: N25.D39
Fix an appointment now and be part of the future of healthcare.